Plasmodium falciparum
| Plasmodium falciparum | |
|---|---|

| |
| Macrogametocyte (left) and microgametocyte (right) of P. falciparum | |
| Scientific classification | |
| Domain: | Eukaryota |
| Clade: | Diaphoretickes |
| Clade: | SAR |
| Clade: | Alveolata |
| Phylum: | Apicomplexa |
| Class: | Aconoidasida |
| Order: | Haemospororida |
| Family: | Plasmodiidae |
| Genus: | Plasmodium |
| Species: | P. falciparum
|
| Binomial name | |
| Plasmodium falciparum (Welch, 1897)
| |
| Synonyms[1] | |
| |
Plasmodium falciparum is a
The species originated from the malarial parasite
In 2022, some 249 million cases of malaria worldwide resulted in an estimated 608000 deaths, with 80 percent being 5 years old or less.[7] Nearly all malarial deaths are caused by P. falciparum, and 95% of such cases occur in Africa. In Sub-Saharan Africa, almost 100% of cases were due to P. falciparum, whereas in most other malarial countries, other, less virulent plasmodial species predominate.[8]
History

Falciparum malaria was familiar to the ancient Greeks, who gave the general name πυρετός (pyretós) "fever".[9] Hippocrates (c. 460–370 BCE) gave several descriptions on tertian fever and quartan fever.[10] It was prevalent throughout the ancient Egyptian and Roman civilizations.[11] It was the Romans who named the disease "malaria"—mala for bad, and aria for air, as they believed that the disease was spread by contaminated air, or miasma.[10][12]
Discovery
A German physician,
The British physician Patrick Manson formulated the mosquito-malaria theory in 1894; until that time, malarial parasites were believed to be spread in air as miasma, a Greek word for pollution.[12] His colleague Ronald Ross of the Indian Medical Service validated the theory while working in India. Ross discovered in 1897 that malarial parasites lived in certain mosquitoes. The next year, he demonstrated that a malarial parasite of birds could be transmitted by mosquitoes from one bird to another. Around the same time, Grassi demonstrated that P. falciparum was transmitted in humans only by female anopheline mosquito (in his case Anopheles claviger).[14] Ross, Manson and Grassi were nominated for the Nobel Prize in Physiology or Medicine in 1902. Under controversial circumstances, only Ross was selected for the award.[15]
There was a long debate on the taxonomy. It was only in 1954 the
Origin and evolution
P. falciparum is now generally accepted to have evolved from
Levels of genetic polymorphism are extremely low within the P. falciparum genome compared to that of closely related, ape infecting species of Plasmodium (including P. praefalciparum).[24][20] This suggests that the origin of P. falciparum in humans is recent, as a single P. praefalciparum strain became capable of infecting humans.[20] The genetic information of P. falciparum has signaled a recent expansion that coincides with the agricultural revolution. It is likely that the development of extensive agriculture increased mosquito population densities by giving rise to more breeding sites, which may have triggered the evolution and expansion of P. falciparum.[25]
Structure


P. falciparum does not have a fixed structure but undergoes continuous change during the course of its life cycle. A sporozoite is spindle-shaped and 10–15 μm long. In the liver it grows into an ovoid schizont of 30–70 μm in diameter. Each schizont produces merozoites, each of which is roughly 1.5 μm in length and 1 μm in diameter. In the erythrocyte the merozoite form a ring-like structure, becoming a trophozoite. A trophozoite feeds on the haemoglobin and forms a granular pigment called
The apical complex, which is actually a combination of organelles, is an important structure. It contains secretory organelles called rhoptries and micronemes, which are vital for mobility, adhesion, host cell invasion, and parasitophorous vacuole formation.
Genome
In 1995 the Malaria Genome Project was set up to sequence the genome of P. falciparum. The genome of its
Life cycle

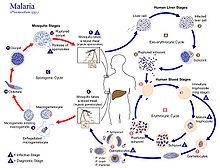
Humans are the intermediate hosts in which asexual reproduction occurs, and female anopheline mosquitos are the definitive hosts harbouring the sexual reproduction stage.[32]
In humans
Infection in humans begins with the bite of an infected female Anopheles mosquito. Out of about 460 species of Anopheles mosquito, more than 70 species transmit falciparum malaria.[33] Anopheles gambiae is one of the best known and most prevalent vectors, particularly in Africa.[34]
The infective stage called the
Liver stage or exo-erythrocytic schizogony
Entering the hepatocytes, the parasite loses its
Blood stage or erythrocytic schizogony
Within the erythrocyte, the parasite metabolism depends on the digestion of
The parasite can also alter the morphology of the erythrocyte, causing knobs on the erythrocyte membrane. Infected erythrocytes are often sequestered in various human tissues or organs, such as the heart, liver and brain. This is caused by parasite-derived cell surface proteins being present on the erythrocyte membrane, and it is these proteins that bind to receptors on human cells. Sequestration in the brain causes cerebral malaria, a very severe form of the disease, which increases the victim's likelihood of death.[42]
Trophozoite
After invading the erythrocyte, the parasite loses its specific invasion organelles (apical complex and surface coat) and de-differentiates into a round trophozoite located within a parasitophorous vacuole. The trophozoite feeds on the haemoglobin of the erythrocyte, digesting its proteins and converting (by
Schizont
At the schizont stage, the parasite replicates its DNA multiple times and multiple mitotic divisions occur asynchronously.[46][47] Cell division and multiplication in the erythrocyte is called erythrocytic schizogony. Each schizont forms 16-18 merozoites.[45] The red blood cells are ruptured by the merozoites. The liberated merozoites invade fresh erythrocytes. A free merozoite is in the bloodstream for roughly 60 seconds before it enters another erythrocyte.[40]
The duration of one complete erythrocytic schizogony is approximately 48 hours. This gives rise to the characteristic clinical manifestations of falciparum malaria, such as fever and chills, corresponding to the synchronous rupture of the infected erythrocytes.[48]
Gametocyte
Some merozoites differentiate into sexual forms, male and female gametocytes. These gametocytes take roughly 7–15 days to reach full maturity, through the process called gametocytogenesis. These are then taken up by a female Anopheles mosquito during a blood meal.[49]
Incubation period
The time of appearance of the symptoms from infection (called incubation period) is shortest for P. falciparum among Plasmodium species. An average incubation period is 11 days,[48] but may range from 9 to 30 days. In isolated cases, prolonged incubation periods as long as 2, 3 or even 8 years have been recorded.[50] Pregnancy and co-infection with HIV are important conditions for delayed symptoms.[51] Parasites can be detected from blood samples by the 10th day after infection (pre-patent period).[48]
In mosquitoes
Within the mosquito midgut, the female gamete maturation process entails slight morphological changes, becoming more enlarged and spherical. The male gametocyte undergoes a rapid nuclear division within 15 minutes, producing eight
Meiosis
Plasmodium falciparum is haploid (one set of chromosomes) during its reproductive stages in human blood and liver. When a mosquito takes a blood meal from a plasmodium infected human host, this meal may include haploid microgametes and macrogametes. Such gametes can fuse within the mosquito to form a diploid (2N) plasmodium zygote, the only diploid stage in the life cycle of these parasites.[54] The zygote can undergo another round of chromosome replication to form a ookinete (4N) (see Figure: Life cycle of plasmodium). The ookinete that differentiates from the zygote is a highly mobile stage that invades the mosquito midgut. The ookinetes can undergo meiosis involving two meiotic divisions leading to the release of haploid sporozoites (see Figure).[54] The sporozoite is an elongated crescent shaped invasive stage. These sporozoites may migrate to the mosquito’s salivary glands and can enter a human host when the mosquito takes a blood meal. The sporozoite then can move to the human host liver and infect hepatocytes.
The profile of genes encoded by plasmodium that are employed in meiosis has some overlap with the profile of genes employed in meiosis in other more well studied organisms, but is more divergent and is lacking some components of the meiotic process found in other organisms.[54] During plasmodium meiosis, recombination occurs between homologous chromosomes as in other organisms.
Interaction with human immune system
Immune response
A single anopheline mosquito can transmit hundreds of P. falciparum sporozoites in a single bite under experimental conditions, but, in nature the number is generally less than 80.
Only a small number (0.5-5%) of sporozoites enter the blood stream into the liver. In the liver, the activated CD8+ T cells from the lymph bind the sporozoites through the
Immune system evasion
Although P. falciparum is easily recognized by the human immune system while in the bloodstream, it evades immunity by producing over 2,000 cell membrane antigens.[60] The initial infective stage sporozoites produce circumsporozoite protein (CSP), which binds to hepatocytes.[61] Binding to and entering into the hepatocytes is aided by thrombospondin-related anonymous protein (TRAP).[62] TRAP and other secretory proteins (including sporozoite microneme protein essential for cell traversal 1, SPECT1 and SPECT2) from microneme allow the sporozoite to move through the blood, avoiding immune cells and penetrating hepatocytes.[63]
During erythrocyte invasion, merozoites release merozoite cap protein-1 (MCP1), apical membrane antigen 1 (AMA1), erythrocyte-binding antigens (EBA), myosin A tail domain interacting protein (MTIP), and
Pathogenicity
The clinical symptoms of falciparum malaria are produced by the rupture and destruction of erythrocytes by the merozoites. High fever, called paroxysm, is the most basic indication. The fever has a characteristic cycle of hot stage, cold stage and sweating stages.
The insoluble β-hematin crystals, haemozoin, produced from digestion of haemoglobin of the RBCs is the main agent that affect body organs. Acting as a blood toxin, haemozoin-containing RBCs cannot be attacked by phagocytes during immune response to malaria.
Unlike other malarias, which show regular periodicity of fever, falciparum, though exhibiting a 48-hour cycle, usually presents as irregular bouts of fever. This difference is due the ability of P. falciparum merozoites to invade a large number of RBCs sequentially without coordinated intervals, which is not seen in other malarial parasites.
P. falciparum works via sequestration, a process by which group of infected RBCs are clustered, which is not exhibited by any other species of malarial parasites.
Cerebral malaria is the most dangerous condition of any malarial infection and the most severe form of
The reappearance of falciparum symptom, a phenomenon called recrudescence, is often seen in survivors.[86] Recrudescence can occur even after successful antimalarial medication.[87][88] It may take a few months or even several years. In some individuals, it takes as along as three years.[89] In isolated cases, the duration can reach or exceed 10 years.[90][91] It is also a common incident among pregnant women.[92][93]
Distribution and epidemiology

P. falciparum is endemic in 84 countries,[95] and is found in all continents except Europe. Historically, it was present in most European countries, but improved health conditions led to the disappearance in the early 20th century.[96] The only European country where it used to be historically prevalent, and from where we got the name malaria, Italy had been declared malaria-eradicated country. In 1947, the Italian government launched the National Malaria Eradication Program, and following, an anti-mosquito campaign was implemented using DDT.[97] The WHO declared Italy free of malaria in 1970.[98]
There were 247 million cases of malaria worldwide in 2021, resulting in an estimated 619,000 deaths.[95] The infection is most prevalent in Africa, where 94% of malaria deaths occur. Children under five years of age are most affected, and 67% of malaria deaths occurred in this age group. 80% of the infection is found in Sub-Saharan Africa, 7% in the South-East Asia, and 2% in the Eastern Mediterranean. Nigeria has the highest incidence, with 27% of the total global cases. Outside Africa, India has the highest incidence, with 4.5% of the global burden. Europe is regarded as a malaria-free region. Historically, the parasite and its disease had been most well known in Europe. But medical programmes since the early 20th century, such as insecticide spraying, drug therapy and environmental engineering, resulted in complete eradication in the 1970s.[99] It is estimated that approximately 2.4 billion people are at constant risk of infection.[100]
Treatment
History
In 1640, Huan del Vego first employed the
Attempts to make synthetic antimalarials began in 1891.
Uncomplicated malaria
According to WHO guidelines 2010,
The choice of ACT is based on the level of resistance to the constituents in the combination. Artemisinin and its derivatives are not appropriate for monotherapy. As second-line antimalarial treatment, when initial treatment does not work, an alternative ACT known to be effective in the region is recommended, such as artesunate plus tetracycline or
Severe malaria
For adults,
For children, especially in the malaria-endemic areas of Africa, artesunate IV or IM, quinine (IV infusion or divided IM injection), and artemether IM are recommended.[106]
Parenteral antimalarials should be administered for a minimum of 24 hours, irrespective of the patient's ability to tolerate oral medication earlier.[106] Thereafter, complete treatment is recommended including complete course of ACT or quinine plus clindamycin or doxycycline.[106]
Vaccination
RTS,S is the only candidate as malaria vaccine to have gone through clinical trials.[107] Analysis of the results of the phase III trial (conducted between 2011 and 2016) revealed a rather low efficacy (20-39% depending on age, with up to 50% in 5–17-month aged babies), indicating that the vaccine will not lead to full protection and eradication.[108]
On October 6, 2021, the World Health Organization recommended malaria vaccination for children at risk.[109]
Cancer
The
In 1989, it was realised that EBV requires other infections such as with malaria to cause lymphocyte transformation. It was reported that the incidence of Burkitt's lymphoma decreased with effective treatment of malaria over several years.
Influence on the human genome
The high
See also
- Malaria Atlas Project
- List of parasites (human)
- UCSC Malaria Genome Browser
References
- ^ Coatney GR, Collins WE, Warren M, Contacos PG (1971). "22 Plasmodium falciparum (Welch, 1897)". The primate malarias. Division of Parasitic Disease, CDC. p. 263.
- PMID 19666593.
- PMID 22110393.
- PMID 11140853.
- ^ PMID 27381764.
- ^ PMID 32905751.
- ^ "World malaria report 2022". www.who.int. Retrieved 2024-01-30.
- ISBN 978-92-4-004049-6.
- S2CID 142602810.
- ^ PMID 23835014.
- )
- ^ a b c Lalchhandama, K. (2014). "The making of modern malariology: from miasma to mosquito- malaria theory" (PDF). Science Vision. 14 (1): 3–17. Archived from the original (PDF) on 2014-04-27.
- PMID 20205846.

- PMID 20055226.
- PMID 16636993.
- ^ PMID 15462972.
- PMID 20781927.
- PMID 20864995.
- S2CID 205058952.
- ^ PMID 20864995.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - PMID 20498054.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - PMID 21354860.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - PMID 11356517.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - S2CID 11020105.
- PMID 12643998.
- ISBN 978-3-527-32848-2.
- PMID 16337634.
- ^ PMID 17041140.
- PMID 21912516.
- PMID 8757284.
- ^ PMID 12368864.
- PMID 31316507.
- PMID 27732796.
- PMID 21129198.
- S2CID 21437365.
- ^ PMID 21317311.
- PMID 14700584.
- PMID 28242785.
- S2CID 22790721.
- ^ S2CID 14972823.
- ^ "Malaria eModule – SYNCHRONICITY".
- PMID 31562653.
- S2CID 4420567.
- S2CID 30446678. Archived from the originalon 2011-06-10.
- ^ a b "Malaria eModule – ASEXUAL ERYTHROCYTIC STAGES".
- S2CID 24655319.
- PMID 20816844.
- ^ PMID 12930555.
- PMID 15253774.
- PMID 22708041.
- PMID 18258132.
- S2CID 27083717.
- PMID 1951866.
- ^ a b c Guttery DS, Zeeshan M, Holder AA, Tromer EC, Tewari R. Meiosis in Plasmodium: how does it work? Trends Parasitol. 2023 Oct;39(10):812-821. doi: 10.1016/j.pt.2023.07.002. Epub 2023 Aug 2. PMID: 37541799
- S2CID 27449694.
- ^ S2CID 17601147.
- PMID 25694058.
- PMID 27799922.
- PMID 12869017.

- ^ S2CID 4412848.
- S2CID 8825913.
- S2CID 30488807.
- PMID 18779047.
- S2CID 7811400.
- .
- ^ PMID 21413352, retrieved 2022-02-01
- PMID 29004267.
- PMID 32288635.
- PMID 33568138.
- PMID 24556123.
- S2CID 45386035.
- PMID 22583751.
- PMID 31571584.
- PMID 24550911.
- PMID 20637890.
- ^ PMID 25015559.
- PMID 24897084.
- PMID 25473835.
- PMID 14744557.
- PMID 11103309.
- PMID 34746025.
- S2CID 847217.
- PMID 11425172.
- S2CID 58560596.
- PMID 20606600.
- PMID 25918217.
- PMID 20863228.
- PMID 26381375.
- PMID 28044045.
- PMID 28719260.
- S2CID 207949553.
- PMID 19134201.
- PMID 26017553.
- PMID 27777030.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ ISBN 978-92-4-006489-8.
- PMID 22550561.
- PMID 2665000.
- PMID 33734023.
- PMID 27172807.
- PMID 21482730.
- PMID 1490916.
- PMID 15669029.
- S2CID 71742454.
- .
- PMID 26481135.
- ^ ISBN 978-92-4-154792-5
- PMID 28500775.
- PMID 28272979.
- ^ "WHO recommends groundbreaking malaria vaccine for children at risk". www.who.int. Retrieved 2021-11-15.
- PMID 26789827.

- PMID 19350698.
- PMID 2923122.
- PMID 25164057.
- PMID 29116588.
- PMID 27956028.

- PMID 26794909.

- PMID 16001361.

- PMID 21427751.

- PMID 21027890.
- PMID 21427751.
- PMID 12149194.
- PMID 17912355.
Further reading
- Colombian scientists develop computational tool to detect Plasmodium falciparum (in Spanish)
- Allison, A.C. (February 1954). "Protection Afforded by Sickle-cell Trait Against Subtertian Malarial Infection". Br Med J. 1 (4857): 290–4. PMID 13115700.
- Allison, AC (1964). "Polymorphism and Natural Selection in Human Populations". Cold Spring Harb. Symp. Quant. Biol. 29: 137–49. PMID 14278460.
- Cholera, R; Brittain NJ; Gillrie MR; et al. (January 2008). "Impaired cytoadherence of Plasmodium falciparum-infected erythrocytes containing sickle hemoglobin". Proc. Natl. Acad. Sci. U.S.A. 105 (3): 991–6. PMID 18192399.
- Mockenhaupt, FP; Ehrhardt, S; Otchwemah, R; et al. (May 2004). "Limited influence of haemoglobin variants on Plasmodium falciparum msp1 and msp2 alleles in symptomatic malaria". Trans. R. Soc. Trop. Med. Hyg. 98 (5): 302–10. PMID 15109555.
- Roberts, Larry S.; Janovy, John (2005). Foundations of Parasitology (7th ed.). McGraw-Hill Education (ISE Editions). ISBN 978-0-07-111271-0.
External links
- Malaria species info at CDC
- Web Atlas of Medical Parasitology
- Species profile at Encyclopedia of Life
- Taxonomy at UniProt
- Profile at Scientists Against Malaria
- Genome info at Wellcome Trust Sanger Institute
- PlasmoDB: The Plasmodium Genome Resource
- UCSC Plasmodium Falciparum Browser
- Gene info at Kyoto University
