CDKN1B
Ensembl | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| UniProt | |||||||||
| RefSeq (mRNA) | |||||||||
| RefSeq (protein) | |||||||||
| Location (UCSC) | Chr 12: 12.69 – 12.72 Mb | Chr 6: 134.9 – 134.9 Mb | |||||||
| PubMed search | [3] | [4] | |||||||
| View/Edit Human | View/Edit Mouse |
Cyclin-dependent kinase inhibitor 1B (p27Kip1) is an
Function
The p27Kip1 gene has a
Regulation
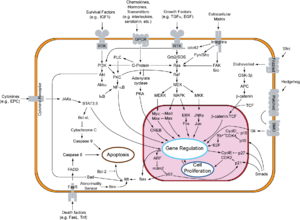
In general, extracellular growth factors which promote cell division reduce transcription and translation of p27Kip1. Also, increased synthesis of CDk4,6/cyclin D causes binding of p27 to this complex, sequestering it from binding to the CDk2/cyclin E complex. Furthermore, an active CDK2/cyclin E complex will phosphorylate p27 and tag p27 for ubiquitination.[7] A mutation of this gene may lead to loss of control over the cell cycle leading to uncontrolled cellular proliferation.[8][9][10] Loss of p27 expression has been observed in metastatic canine mammary carcinomas.[11][12][13] Decreased TGF-beta signalling has been suggested to cause loss of p27 expression in this tumor type.[14]
A
P27 regulation is accomplished by two different mechanisms. In the first its concentration is changed by the individual rates of transcription, translation, and proteolysis. P27 can also be regulated by changing its subcellular location [16] Both mechanisms act to reduce levels of p27, allowing for the activation of Cdk1 and Cdk2, and for the cell to begin progressing through the cell cycle.
Transcription
Transcription of the CDKN1B gene is activated by Forkhead box class O family (FoxO) proteins which also acts downstream to promote p27 nuclear localization and decrease levels of COP9 subunit 5(COPS5) which helps in the degradation of p27.[17] Transcription for p27 is activated by FoxO in response to cytokines, promyelocytic leukaemia proteins, and nuclear Akt signaling.[17] P27 transcription has also been linked to another tumor suppressor gene, MEN1, in pancreatic islet cells where it promotes CDKN1B expression.[17]
Translation
Translation of CDKN1B reaches its maximum during quiescence and early G1.[17] Translation is regulated by polypyrimidine tract-binding protein(PTB), ELAVL1, ELAVL4, and microRNAs.[17] PTB acts by binding CDKN1b IRES to increase translation and when PTB levels decrease, G1 phase is shortened.[17] ELAVL1 and ELAVL4 also bind to CDKN1B IRES but they do so in order to decrease translation and so depletion of either results in G1 arrest.[17]
Proteolysis
Degradation of the p27 protein occurs as cells exit quiescence and enter G1.[17] Protein levels continue to fall rapidly as the cell continues through G1 and enters S phase. One of the most understood mechanisms for p27 proteolysis is the polyubiquitylation of p27 by the SCFSKP2 kinase associated protein 1 (Skp1) and 2 (Skp2).[17] SKP1 and Skp2 degrades p27 after it has been phosphorylated at threonine 187 (Thr187) by either activating cyclin E- or cyclin A-CDK2. Skp2 is mainly responsible for the degradation of p27 levels that continues through S phase.[18] However it is rarely expressed in early G1 where p27 levels first begin to decrease. During early G1 proteolysis of p27 is regulated by KIP1 Ubiquitylation Promoting Complex (KPC) which binds to its CDK inhibitory domain.[19] P27 also has three Cdk-inhibited tyrosines at residues 74, 88, and 89.[17] Of these, Tyr74 is of special interest because it is specific to p27-type inhibitors.[17]
Nuclear export
Alternatively to the transcription, translation, and proteolytic method of regulation, p27 levels can also be changed by exporting p27 to the cytoplasm. This occurs when p27 is phosphorylated on Ser(10) which allows for CRM1, a nuclear export carrier protein, to bind to and remove p27 from the nucleus.[20] Once p27 is excluded from the nucleus it cannot inhibit the cell's growth. In the cytoplasm it may be degraded entirely or retained.[16] This step occurs very early when the cell is exiting the quiescent phase and thus is independent of Skp2 degradation of p27.[20]
MicroRNA regulation
Because p27 levels can be moderated at the translational level, it has been proposed that p27 may be regulated by miRNAs. Recent research has suggested that both miR-221 and miR-222 control p27 levels although the pathways are not well understood.[16]
Role in cancer
Proliferation
p27 is considered a tumor suppressor because of its function as a regulator of the cell cycle.
Metastasis
In cancer cells, p27 can also be mislocalized to the cytoplasm in order to facilitate metastasis. The mechanisms by which it acts on motility differ between cancers. In hepatocellular carcinoma cells p27 co-localizes with actin fibers to act on GTPase Rac and induce cell migration.[22] In breast cancer cytoplasmic p27 reduced RHOA activity which increased a cell's propensity for motility.[23]
This role for p27 may indicate why cancer cells rarely fully inactivate or delete p27. By retaining p27 in some capacity it can be exported to the cytoplasm during tumorigenesis and manipulated to aid in metastasis. 70% of metastatic melanomas were shown to exhibit cytoplasmic p27, while in benign melanomas p27 remained localized to the nucleus.[24] P27 is misplaced to the cytoplasm by the MAP2K, Ras, and Akt pathways although the mechanisms are not entirely understood.[25][26][27] Additionally, phosphorylation of p27 at T198 by RSK1 has been shown to mislocalize p27 to the cytoplasm as well as inhibit the RhoA pathway.[28] Because inhibition of RhoA results in a decrease in both stress fibers and focal adhesion, cell motility is increased.[29] P27 can also be exported to the cytoplasm by oncogenic activation of the P13K pathway.[29] Thus, mislocalization of p27 to the cytoplasm in cancer cells allows them to proliferate unchecked and provides for increased motility.
In contrast to these results, p27 has also been shown to be an inhibitor of migration in sarcoma cells.[30] In these cells, p27 bound to stathmin which prevents stathmin from binding to tubulin and thus polymerization of microtubules increased and cell motility decreased.[30]
MicroRNA regulation
Studies of various cell lines including glioblastoma cell lines, three prostate cancer cell lines, and a breast tumor cell line showed that suppressing miR-221 and miR-22 expression resulted in p27-dependent G1 growth arrest[16] Then when p27 was knocked down, cell growth resumed indicating a strong role for miRNA regulated p27.[16] Studies in patients have demonstrated an inverse correlation between miR-221&22 and p27 protein levels. Additionally nearby healthy tissue showed high expression of the p27 protein while miR-221&22 concentrations were low.[16]
Regulation in specific cancers
In most cancers reduced levels of nuclear p27 are correlated with increased tumor size, increased tumor grade, and a higher propensity for metastasis. However the mechanisms by which levels of p27 are regulated vary between cancers.
Breast
In breast cancer, Src activation has been shown to correlate with low levels of p27[21] Breast cancers that were Estrogen receptor negative and progesterone receptor negative were more likely to display low levels of p27 and more likely to have a high tumor grade.[21] Similarly, breast cancer patients with BRCA1/2 mutations were more likely to have low levels of p27.[31]
Prostate
A mutation in the CDKN1B gene has been linked to an increased risk for hereditary prostate cancer in humans.[32]
Multiple Endocrine Neoplasia
Mutations in the CDKN1B gene has been reported in families affected by the development of
Clinical significance
Prognostic value
Several studies have demonstrated that reduced p27 levels indicate a poorer patient prognosis.[17] However, because of the dual, contrasting roles p27 plays in cancer (as an inhibitor of growth and as a mechanism for metastasis) low levels of p27 may demonstrate that a cancer is not aggressive and will remain benign.[17] In ovarian cancer, p27 negative tumors progressed in 23 months compared to 85 months in p27 positive tumors and thus could be used as a prognostic marker.[34] Similar studies have correlated low levels of p27 with a worse prognosis in breast cancer.[35] Colorectal carcinomas that lacked p27 were shown to have increased p27-specific proteolysis and a median survival of only 69 months compared to 151 months for patients with high or normal levels of p27.[36] The authors proposed clinicians could use patient specific levels of p27 to determine who would benefit from adjuvant therapy.[36] Similar correlations were observed in patients with non-small cell lung cancer,[37] those with colon,[37] and prostate cancer.[38]
So far studies have only evaluated the prognostic value of p27 retrospectively and a standardized scoring system has not been established.[17] However it has been proposed that clinicians should evaluate a patient's p27 levels in order to determine if they will be responsive to certain chemotoxins which target fast growing tumors where p27 levels are low.[17] Or in contrast, if p27 levels are found to be high in a patient's cancer, their risk for metastasis is higher and the physician can make an informed decision about their treatment plan.[17] Because p27 levels are controlled post-transcriptionally, proteomic surveys can be used to establish and monitor a patient's individual levels which aids in the future of individualized medicine.
The following cancers have been demonstrated to have an inverse correlation with p27 expression and prognosis: oro-pharyngo-laryngeal, oesophageal, gastric, colon, lung, melanoma, glioma, breast cancer, prostate, lymphoma, leukemia.[18]
Correlation to treatment response
P27 may also allow clinicians to better select an appropriate treatment for a patient. For example, patients with non-small cell lung cancer who were treated with platinum based chemotherapy showed reduced survival if they had low levels of p27.[39] Similarly low levels of p27 correlated with poor results from adjuvant chemotherapy in breast cancer patients.[40]
Value as a therapeutic target
P27 has been explored as a potential target for cancer therapy because its levels are highly correlated to patient prognosis.[41] This is true for a wide spectrum of cancers including colon, breast, prostate, lung, liver, stomach, and bladder.[41]
Use of microRNAs for therapy
Because of the role miRNAs play in p27 regulation, research is underway to determine if antagomiRs that block the activity of the miR221&222 and allow for p27 cell grow inhibition to take place could act as therapeutic cancer drugs.[16]
Role in Regeneration
Knockdown of CDKN1B stimulates regeneration of cochlear hair cells in mice. Since CDKN1B prevents cells from entering the cell cycle, inhibition of the protein could cause re-entry and subsequent division. In mammals where regeneration of cochlear hair cells normally does not occur, this inhibition could help regrow damaged cells who are otherwise incapable of proliferation. In fact, when the CDKN1B gene is disrupted in adult mice, hair cells of the organ of Corti proliferate, while those in control mice do not. Lack of CDKN1B expression appears to release the hair cells from natural cell-cycle arrest.[42][43] Because hair cell death in the human cochlea is a major cause of hearing loss, the CDKN1B protein could be an important factor in the clinical treatment of deafness.
Interactions
CDKN1B has been shown to
See also
- Sic1 (homologue in Saccharomyces cerevisiae)
- P21waf-1 (another CDK inhibitor)
- Hyaluronic acid synthase
- Hyaluronidase
References
- ^ a b c GRCh38: Ensembl release 89: ENSG00000111276 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000003031 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- S2CID 38513201.
- PMID 11250752.
- ISBN 978-0-87893-300-6.
- S2CID 15490866.
- S2CID 19030818.
- S2CID 2009281.
- PMID 19185891.
- PMID 19748645.
- S2CID 206509356.
- PMID 19836277.
- PMID 12837699.
- ^ S2CID 22887986.
- ^ S2CID 2175257.
- ^ S2CID 19594293.
- PMID 15746103.
- ^ PMID 11889117.
- ^ PMID 17254967.
- PMID 12482975.
- PMID 16489017.
- PMID 17909030.
- PMID 9448290.
- S2CID 23027631.
- S2CID 6580033.
- PMID 19470470.
- ^ PMID 19829074.
- ^ PMID 15652749.
- PMID 11118465.
- PMID 15026335.
- PMID 28824003.)
{{cite journal}}: CS1 maint: DOI inactive as of February 2024 (link - PMID 10446997.
- S2CID 25460889.
- ^ S2CID 3164478.
- ^ PMID 9270000.
- PMID 9458103.
- PMID 10767357.
- PMID 17148774.
- ^ PMID 12620406.
- PMID 10097167.
- PMID 25278894.
- ^ PMID 12042314.
- ^ PMID 12813041.
- ^ PMID 12140288.
- ^ S2CID 25204152.
- S2CID 4427026.
- S2CID 45094232.
- ^ PMID 12529437.
- PMID 9891079.
- ^ PMID 12972555.
- S2CID 42766325.
- PMID 12417722.
- PMID 15355997.
- PMID 10908655.
- PMID 11278754.
- PMID 10891500.
- PMID 11889117.
Further reading
- Marone M, Bonanno G, Rutella S, Leone G, Scambia G, Pierelli L (2003). "Survival and cell cycle control in early hematopoiesis: role of bcl-2, and the cyclin dependent kinase inhibitors P27 and P21". Leuk. Lymphoma. 43 (1): 51–7. S2CID 28490341.
- Hirabayashi H (2003). "[P27 expression and survival in NSCLC]". Nippon Rinsho. 60 (Suppl 5): 263–6. PMID 12101669.
- Bloom J, Pagano M (2003). "Deregulated degradation of the cdk inhibitor p27 and malignant transformation". Semin. Cancer Biol. 13 (1): 41–7. PMID 12507555.
- Tokumoto M, Tsuruya K, Fukuda K, Kanai H, Kuroki S, Hirakata H, Iida M (2003). "Parathyroid cell growth in patients with advanced secondary hyperparathyroidism: vitamin D receptor and cyclin-dependent kinase inhibitors, p21 and p27". Nephrol. Dial. Transplant. 18 (Suppl 3): iii9–iii12. PMID 12771291.
- Drexler HC (2004). "The role of p27Kip1 in proteasome inhibitor induced apoptosis". Cell Cycle. 2 (5): 438–41. S2CID 86142010.
- Le XF, Pruefer F, Bast RC (2006). "HER2-targeting antibodies modulate the cyclin-dependent kinase inhibitor p27Kip1 via multiple signaling pathways". Cell Cycle. 4 (1): 87–95. PMID 15611642.
- Belletti B, Nicoloso MS, Schiappacassi M, Chimienti E, Berton S, Lovat F, Colombatti A, Baldassarre G (2005). "p27(kip1) functional regulation in human cancer: a potential target for therapeutic designs". Curr. Med. Chem. 12 (14): 1589–605. PMID 16022660.
- Sankaranarayanan P, Schomay TE, Aiello KA, Alter O (April 2015). "Tensor GSVD of Patient- and Platform-Matched Tumor and Normal DNA Copy-Number Profiles Uncovers Chromosome Arm-Wide Patterns of Tumor-Exclusive Platform-Consistent Alterations Encoding for Cell Transformation and Predicting Ovarian Cancer Survival". PLOS ONE. 10 (4): e0121396. PMID 25875127.
External links
- CDKN1B human gene location in the UCSC Genome Browser.
- CDKN1B human gene details in the UCSC Genome Browser.
- Overview of all the structural information available in the PDB for UniProt: P46527 (Cyclin-dependent kinase inhibitor 1B) at the PDBe-KB.

