Sinusitis
| Sinusitis | |
|---|---|
| Other names | Sinus infection, rhinosinusitis |
| Frequency | 10–30% each year (developed world)[1][7] |
Sinusitis, also known as rhinosinusitis, is an inflammation of the mucous membranes that line the sinuses resulting in symptoms that may include thick nasal mucus, a plugged nose, and facial pain.[1][8]
Sinusitis usually occurs in individuals with underlying conditions
Some cases may be prevented by hand washing,
Sinusitis is a common condition.[1] It affects between about 10 and 30 percent of people each year in the United States and Europe.[1][7] Chronic sinusitis affects about 12.5% of people.[14] Treatment of sinusitis in the United States results in more than US$11 billion in costs.[1] The unnecessary and ineffective treatment of viral sinusitis with antibiotics is common.[1]
Signs and symptoms
Headache, facial pain, or pressure of a dull, constant, or aching sort over the affected sinuses is common with both acute and chronic stages of sinusitis. This pain is usually localized to the involved sinus and may worsen when the affected person bends over or lies down. Pain often starts on one side of the head and progresses to both sides.[15] Acute sinusitis may be accompanied by a thick nasal discharge that is usually green in color, and may contain pus or blood.[16] Often, a localized headache or toothache is present, and these symptoms distinguish a sinus-related headache from other types of headaches, such as tension and migraine headaches. Another way to distinguish between toothache and sinusitis is that the pain in sinusitis is usually worsened by tilting the head forward and with the Valsalva maneuver.[17]
Other symptoms associated with acute rhinosinusitis include cough, fatigue, hyposmia, anosmia and ear fullness or pressure.[18]
Sinus infections can also cause middle-ear problems due to the congestion of the nasal passages. This can be demonstrated by dizziness, "a pressurized or heavy head", or vibrating sensations in the head.
A 2005 review suggested that most "sinus headaches" are migraines.
Symptoms of
By location
The four paired paranasal sinuses are the frontal, ethmoidal, maxillary, and sphenoidal sinuses. The ethmoidal sinuses are further subdivided into anterior and posterior ethmoid sinuses, the division of which is defined as the basal lamella of the middle nasal concha. In addition to the severity of disease, discussed below, sinusitis can be classified by the sinus cavity it affects:
- Maxillary – can cause pain or pressure in the maxillary (cheek) area (e.g., toothache,[17] or headache) (J01.0/J32.0)
- Frontal – can cause pain or pressure in the frontal sinus cavity (located above the eyes), headache, particularly in the forehead (J01.1/J32.1)
- Ethmoidal – can cause pain or pressure pain between/behind the eyes, the sides of the upper part of the nose (the medial canthi), and headaches (J01.2/J32.2)[23]
- mastoid processes, or the back of the head.[23]
Complications
| Stage | Description |
|---|---|
| I | Preseptal cellulitis |
| II | Orbital cellulitis |
| III | Subperiosteal abscess |
| IV | Orbital abscess |
| V | Cavernous sinus septic thrombosis |
Complications are thought to be rare (1 case per 10,000).[24]
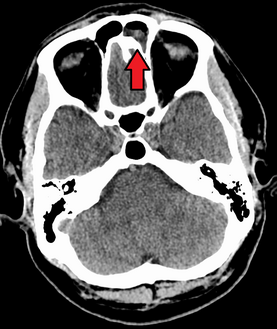
The proximity of the brain to the sinuses makes the most dangerous complication of sinusitis, particularly involving the frontal and sphenoid sinuses, infection of the brain by the invasion of
Sinus infection can spread through
The diagnosis of these complications can be assisted by noting local tenderness and dull pain, and can be confirmed by
If an odontogenic infection or a complication of a dentistry procedure involves the maxillary sinus, odontogenic sinusitis (ODS) may ensue.[33] Odontogenic sinusitis can often spread to other sinuses such as the ethmoid, frontal and (less frequently) sphenoid sinus, and even to the contralateral nasal cavity.[34] In rare instances, these infections may involve the orbit, causing orbital cellulitis, which may in turn result in blindness, or determine central nervous system complications such as meningitis, subdural empyema, brain abscess and life-threatening cavernous sinus thrombosis.[35][36]
Infection of the eye socket is a rare complication of ethmoid sinusitis, which may result in the loss of sight and is accompanied by fever and severe illness. Another possible complication is the infection of the bones (osteomyelitis) of the forehead and other facial bones – Pott's puffy tumor.[15]
Voice box can also get infected resulting in laryngitis.[4][unreliable medical source?] This can result in hoarseness, change in voice, pain in throat, pain while talking, inaudible voice, dry cough and fever.[4][unreliable medical source?]
Causes
Acute
Chronic
By definition, chronic sinusitis lasts longer than 12 weeks and can be caused by many different diseases that share chronic inflammation of the sinuses as a common symptom. It is subdivided into cases with and without
Chronic rhinosinusitis represents a multifactorial inflammatory disorder, rather than simply a persistent bacterial infection.[24] The medical management of chronic rhinosinusitis is now focused upon controlling the inflammation that predisposes people to obstruction, reducing the incidence of infections.[40] Surgery may be needed if medications are not working.[40]
Attempts have been made to provide a more consistent nomenclature for subtypes of chronic sinusitis. The presence of
A more recent, and still debated, development in chronic sinusitis is the role that
Recent theories of sinusitis indicate that it often occurs as part of a spectrum of diseases that affect the respiratory tract (i.e., the "one airway" theory) and is often linked to asthma.[44][45]
Both smoking and
Other diseases such as cystic fibrosis and granulomatosis with polyangiitis can also cause chronic sinusitis.[46]
Maxillary sinus
An estimated 0.5 to 2.0% of viral rhinosinusitis (VRS) will develop into bacterial infections in adults and 5 to 10% in children.[18]
Pathophysiology
Diagnosis
Classification

Sinusitis (or rhinosinusitis) is defined as an inflammation of the mucous membrane that lines the paranasal sinuses and is classified chronologically into several categories:[22]
- Acute sinusitis – A new infection that may last up to four weeks and can be subdivided symptomatically into severe and nonsevere. Some use definitions up to 12 weeks.[1]
- Recurrent acute sinusitis – Four or more full episodes of acute sinusitis that occur within one year
- Subacutesinusitis – An infection that lasts between four and 12 weeks, and represents a transition between acute and chronic infection.
- Chronic sinusitis – When the signs and symptoms last for more than 12 weeks.[1]
- Acute exacerbation of chronic sinusitis – When the signs and symptoms of chronic sinusitis exacerbate, but return to baseline after treatment.
Roughly 90% of adults have had sinusitis at some point in their lives.[52]
Acute
Health care providers distinguish bacterial and viral sinusitis by watchful waiting.[1] If a person has had sinusitis for fewer than 10 days without the symptoms becoming worse, then the infection is presumed to be viral.[1] When symptoms last more than 10 days or get worse in that time, then the infection is considered bacterial sinusitis.[53] Pain in the teeth and bad breath are also more indicative of bacterial disease.[54]
Imaging by either X-ray, CT or MRI is generally not recommended unless complications develop.[53] Pain caused by sinusitis is sometimes confused for pain caused by pulpitis (toothache) of the maxillary teeth, and vice versa. Classically, the increased pain when tilting the head forwards separates sinusitis from pulpitis.[citation needed]
For cases of maxillary sinusitis, limited field
Chronic
For sinusitis lasting more than 12 weeks, a
Nasal
Sinus infections, if they result in tooth pain, usually present with pain involving more than one of the upper teeth, whereas a toothache usually involves a single tooth. Dental examination and appropriate radiography aid in ruling out pain arises from a tooth.[32]
-
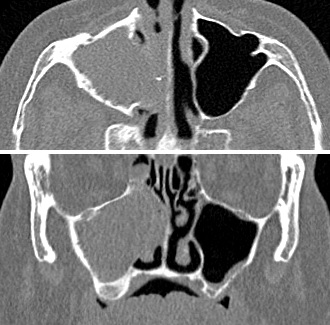
CT of chronic sinusitis
-
CT scan of chronic sinusitis, showing a filled right maxillary sinus with sclerotic thickened bone.
-
MRI image showing sinusitis. Edema and mucosal thickening appears in both maxillary sinuses.
-
Maxillary sinusitis caused by a dental infection associated with periorbital cellulitis
-
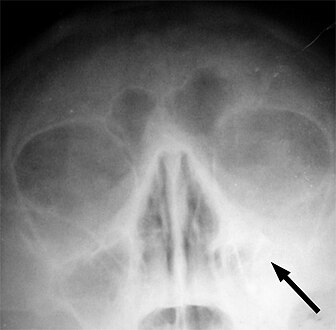
Frontal sinusitis
-
X-ray of left-sided maxillary sinusitis marked by an arrow. There is lack of the air transparency indicating fluid in contrast to the other side.
Treatment
| Treatment | Indication | Rationale |
|---|---|---|
| Time | Viral and some bacterial sinusitis | Sinusitis is usually caused by a virus which is not affected by antibiotics.[57] |
| Antibiotics | Bacterial sinusitis | Cases accompanied by extreme pain, skin infection, or which last a long time may be caused by bacteria.[57] |
| Nasal irrigation | Nasal congestion | Can provide relief by helping decongest.[57] |
| Drink liquids | Thick phlegm | Remaining hydrated loosens mucus.[57] |
Antihistamines
|
Concern with allergies
|
Antihistamines do not relieve typical sinusitis or cold symptoms much; this treatment is not needed in most cases.[57] |
| Nasal spray | Desire for temporary relief | Tentative evidence that it helps symptoms.[6] Does not treat cause. Not recommended for more than three days' use.[57] |
Recommended treatments for most cases of sinusitis include rest and drinking enough water to thin the mucus.[59] Antibiotics are not recommended for most cases.[59][60]
Breathing low-temperature steam such as from a hot shower or
Antibiotics
Most sinusitis cases are caused by viruses and resolve without antibiotics.
A short-course (3–7 days) of antibiotics seems to be just as effective as the typical longer-course (10–14 days) of antibiotics for those with clinically diagnosed acute bacterial sinusitis without any other severe disease or complicating factors.[71] The IDSA guideline suggest five to seven days of antibiotics is long enough to treat a bacterial infection without encouraging resistance. The guidelines still recommend children receive antibiotic treatment for ten days to two weeks.[69]
Corticosteroids
For unconfirmed acute sinusitis, nasal sprays using corticosteroids have not been found to be better than a placebo either alone or in combination with antibiotics.[72] For cases confirmed by radiology or nasal endoscopy, treatment with intranasal corticosteroids alone or in combination with antibiotics is supported.[73] The benefit, however, is small.[74]
For confirmed chronic rhinosinusitis, there is limited evidence that intranasal steroids improve symptoms and insufficient evidence that one type of steroid is more effective.[75][76]
There is only limited evidence to support short treatment with corticosteroids by mouth for chronic rhinosinusitis with nasal polyps.[77][78][79] There is limited evidence to support corticosteroids by mouth in combination with antibiotics for acute sinusitis; it has only short-term effect improving the symptoms.[80][81]
Surgery
For sinusitis of dental origin, treatment focuses on removing the infection and preventing reinfection, by removal of the microorganisms, their byproducts, and pulpal debris from the infected root canal.[36] Systemic antibiotics are ineffective as a definitive solution, but may afford temporary relief of symptoms by improving sinus clearing, and may be appropriate for rapidly spreading infections, but debridement and disinfection of the root canal system at the same time is necessary. Treatment options include non-surgical root canal treatment, periradicular surgery, tooth replantation, or extraction of the infected tooth.[36]
For chronic or recurring sinusitis, referral to an
A number of surgical approaches can be used to access the sinuses and these have generally shifted from external/extranasal approaches to intranasal
Another recently developed treatment is
Treatments directed to rhinovirus infection
A study has shown that patients given spray formulation of 0.73 mg of Tremacamra (a soluble intercellular adhesion molecule 1 [ICAM-1] receptor) reduced the severity of illness.[37]
Prognosis
A 2018 review has found that without the use of antibiotics, about 46% were cured after one week and 64% after two weeks.[66]
Epidemiology
Sinusitis is a common condition, with between 24 and 31 million cases occurring in the United States annually.[89][90] Chronic sinusitis affects approximately 12.5% of people.[14]
Research
Based on recent theories on the role that
See also
References
- ^ S2CID 206469424.
- ^ a b c d e "Sinus Infection (Sinusitis)". cdc.gov. September 30, 2013. Archived from the original on 7 April 2015. Retrieved 6 April 2015.
- ^ Koralla DR (2021-06-27). "Sinus infection symptoms | Problems with sinuses". MedyBlog. Archived from the original on 2022-12-12. Retrieved 2022-12-13.[unreliable medical source?]
- ^ a b c Meghanadh DK (2022-11-18). "Complications of Sinusitis". Medy Blog. Archived from the original on 2023-01-09. Retrieved 2023-01-09.[unreliable medical source?]
- ^ "Migraines vs. Sinus Headaches". American Migraine Foundation. Archived from the original on 2017-07-28. Retrieved 2017-10-23.
- ^ (PDF) from the original on 2021-08-29. Retrieved 2018-04-20.
- ^ ISBN 9780323085939. Archivedfrom the original on 2016-06-03.
- (PDF) from the original on 2018-07-22. Retrieved 2019-09-17.
- ^ a b Meghanadh DK (2022-11-14). "What causes sinusitis infection?". Medy Blog. Archived from the original on 2022-12-12. Retrieved 2022-12-13.[unreliable medical source?]
- ^ a b Meghanadh DK (2022-11-16). "Sinusitis Diagnosis - How to identify it?". Medy Blog. Archived from the original on 2022-12-12. Retrieved 2022-12-13.[unreliable medical source?]
- ^ (PDF) from the original on 2023-03-07. Retrieved 2023-01-21.
- ^ "How Is Sinusitis Treated?". April 3, 2012. Archived from the original on 5 April 2015. Retrieved 6 April 2015.
- ^ Meghanadh DK (2022-12-05). "Treatment for Sinusitis- Acute, Chronic & Subacute stages". Medy Blog. Archived from the original on 2022-12-13. Retrieved 2022-12-13.[unreliable medical source?]
- ^ PMID 21890184.
- ^ a b c "Sinusitus Complications". Patient Education. University of Maryland. Archived from the original on 2010-02-22.
- ^ "Sinusitis". herb2000.com. Archived from the original on 2011-05-25.
Incidence of acute sinusitis almost always set in following the appearance of a cold for several days at a stretch in the person to the point that all the profuse nasal discharge turns a distinct yellow or a dark green color, or perhaps very thick, and foul-smelling in some cases.
[unreliable medical source?] - ^ PMID 24861778.
- ^ PMID 31613481..
 Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License Archived 2017-10-16 at the Wayback Machine
Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License Archived 2017-10-16 at the Wayback Machine - ^ "Chronic Sinusitis". Cleveland Clinic. Archived from the original on 2023-09-26. Retrieved 2023-09-11.
- S2CID 40427174.
- PMID 14979299.
- ^ a b c Radojicic C. "Sinusitis". Disease Management Project. Cleveland Clinic. Archived from the original on November 14, 2012. Retrieved November 26, 2012.
- ^ ISBN 978-0-8138-2131-3.
- ^ PMID 18206715.
- S2CID 32773653.
- S2CID 13223135.
- S2CID 42926700.
- S2CID 33112170.
- PMID 8127580.
- PMID 7742444.
- PMID 7692375.
- ^ OCLC 903962852.
- PMID 33583151.
- from the original on 2024-02-25. Retrieved 2021-03-27.
- ISBN 978-0-323-04903-0.
- ^ a b c d e f "Maxillary Sinusitis of Endodontic Origin" (PDF). American Association of Endodontists. 2018. Archived (PDF) from the original on 26 March 2019. Retrieved 26 March 2019.
- ^ S2CID 201117207.
- ^ Mucormycosis at eMedicine
- OCLC 862758150.
- ^ PMID 21735433.
- PMID 19544383.
- ^ Boodman SG (1999-11-23). "Mayo Report on Sinusitis Draws Skeptics". The Washington Post. Archived from the original on 2019-03-06. Retrieved 2018-06-01.
- PMID 19532095.
- PMID 9042022.
- S2CID 7490538.
- S2CID 5606258.
- PMID 16326178.
- S2CID 46197466.
- S2CID 7259509.
- ISBN 978-0-8247-0635-7. Archivedfrom the original on 2014-01-07.
- S2CID 25830188.
- S2CID 23638755.
- ^ S2CID 16593182.
- PMID 30858261.
- ISBN 9780323080873.
- ^ Harrison's Manual of Medicine 16/e
- ^ ABIM Foundation. Consumer Reports. Archived(PDF) from the original on June 11, 2012. Retrieved August 17, 2012.
- ABIM Foundation. American Academy of Allergy, Asthma, and Immunology. Archived(PDF) from the original on November 3, 2012. Retrieved August 14, 2012.
- ^ ABIM Foundation, Consumer Reports, archived(PDF) from the original on January 24, 2013, retrieved August 14, 2012
- PMID 30198548.
- PMID 17636843.
- ^ Rhinitis medicamentosa at eMedicine
- PMID 25347280.
- PMID 29750825.
- PMID 30199594.
- ^ PMID 30198548.
- PMID 22450938.
- PMID 18362380.
- ^ PMID 22438350.
- ^ "Fluoroquinolone Antibacterial Drugs: Drug Safety Communication – FDA Advises Restricting Use for Certain Uncomplicated Infections". FDA. 12 May 2016. Archived from the original on 16 May 2016. Retrieved 16 May 2016.
- PMID 19154447.
- PMID 18056902.
- PMID 24293353.
- PMID 22585889.
- from the original on 2019-11-15. Retrieved 2019-11-15.
- S2CID 205210689.
- PMID 27113367.
- ^ S2CID 35987497.
- PMID 18438594.
- (PDF) from the original on 2019-11-15. Retrieved 2019-11-15.
- S2CID 205210682.
- ^ Meghanadh DK (2022-12-16). "Fungal sinusitis - causes, symptoms, and treatment". Medy Blog. Archived from the original on 2023-05-05. Retrieved 2023-05-05.[unreliable medical source?]
- ^ Tichenor WS (2007-04-22). "FAQ — Sinusitis". Archived from the original on 2007-11-01. Retrieved 2007-10-28.
- PMID 25437000.
- PMID 25410644.
- S2CID 34575985.
- ^ a b Meghanadh DK (2023-02-07). "Sinusitis Surgery: An Overview of the Different Technologies". Medy Blog. Archived from the original on 2023-05-05. Retrieved 2023-05-05.[unreliable medical source?]
- PMID 23525506.
- PMID 20350632.
- PMID 20176255.
External links
- Sinusitis at Curlie
- "Sinusitis". MedlinePlus. U.S. National Library of Medicine.