COVID-19
- Afrikaans
- አማርኛ
- अंगिका
- Ænglisc
- العربية
- Aragonés
- Armãneashti
- Arpetan
- অসমীয়া
- Asturianu
- Atikamekw
- अवधी
- Avañe'ẽ
- Авар
- Azərbaycanca
- تۆرکجه
- বাংলা
- Banjar
- 閩南語 / Bân-lâm-gú
- Беларуская
- Беларуская (тарашкевіца)
- भोजपुरी
- Bikol Central
- Български
- བོད་ཡིག
- Bosanski
- Brezhoneg
- Буряад
- Català
- Чӑвашла
- Čeština
- Chi-Chewa
- ChiShona
- ChiTumbuka
- Cymraeg
- Dagbanli
- Dansk
- الدارجة
- Deutsch
- ދިވެހިބަސް
- ཇོང་ཁ
- Eesti
- Ελληνικά
- Emiliàn e rumagnòl
- Español
- Esperanto
- Euskara
- فارسی
- Fiji Hindi
- Français
- Frysk
- Fulfulde
- Gaeilge
- Gaelg
- Galego
- 贛語
- Gĩkũyũ
- ગુજરાતી
- Gungbe
- 客家語/Hak-kâ-ngî
- 한국어
- Hausa
- Hawaiʻi
- Հայերեն
- हिन्दी
- Hrvatski
- Bahasa Hulontalo
- Ido
- Bahasa Indonesia
- Interlingua
- ᐃᓄᒃᑎᑐᑦ / inuktitut
- IsiZulu
- Íslenska
- Italiano
- עברית
- Jawa
- ಕನ್ನಡ
- ქართული
- कॉशुर / کٲشُر
- Қазақша
- Kreyòl ayisyen
- Kurdî
- Кыргызча
- ລາວ
- Latina
- Latviešu
- Lëtzebuergesch
- Lietuvių
- Limburgs
- Lingála
- Lombard
- Magyar
- मैथिली
- Македонски
- മലയാളം
- Māori
- मराठी
- მარგალური
- مصرى
- ဘာသာမန်
- مازِرونی
- Bahasa Melayu
- ꯃꯤꯇꯩ ꯂꯣꯟ
- Minangkabau
- 閩東語 / Mìng-dĕ̤ng-ngṳ̄
- Монгол
- မြန်မာဘာသာ
- Nederlands
- Nedersaksies
- नेपाली
- 日本語
- Nordfriisk
- Norsk bokmål
- Norsk nynorsk
- Nouormand
- Occitan
- Олык марий
- ଓଡ଼ିଆ
- Oʻzbekcha / ўзбекча
- ਪੰਜਾਬੀ
- Pangcah
- پنجابی
- ပအိုဝ်ႏဘာႏသာႏ
- Papiamentu
- پښتو
- ភាសាខ្មែរ
- Pinayuanan
- Plattdüütsch
- Polski
- Português
- Qırımtatarca
- Română
- Rumantsch
- Runa Simi
- Русский
- Саха тыла
- Sakizaya
- ᱥᱟᱱᱛᱟᱲᱤ
- Sardu
- Scots
- Seediq
- Sesotho
- Shqip
- සිංහල
- Simple English
- سنڌي
- SiSwati
- Slovenčina
- Slovenščina
- Словѣньскъ / ⰔⰎⰑⰂⰡⰐⰠⰔⰍⰟ
- Ślůnski
- کوردی
- Српски / srpski
- Srpskohrvatski / српскохрватски
- Sunda
- Suomi
- Svenska
- Tagalog
- தமிழ்
- Taqbaylit
- Татарча / tatarça
- ၽႃႇသႃႇတႆး
- Tayal
- తెలుగు
- Tetun
- ไทย
- Thuɔŋjäŋ
- Lea faka-Tonga
- ᏣᎳᎩ
- ತುಳು
- Türkçe
- Türkmençe
- Tyap
- Basa Ugi
- Українська
- اردو
- ئۇيغۇرچە / Uyghurche
- Vahcuengh
- Tiếng Việt
- Walon
- Wayuunaiki
- 文言
- Winaray
- 吴语
- Xitsonga
- Yorùbá
- 粵語
- Zazaki
- 中文
- Fɔ̀ngbè
- ⵜⴰⵎⴰⵣⵉⵖⵜ ⵜⴰⵏⴰⵡⴰⵢⵜ
| Coronavirus disease 2019 (COVID-19) | |
|---|---|
| Other names | COVID, (the) coronavirus |
Symptomatic and supportive | |
| Frequency | 775,293,616[4] confirmed cases (true case count is expected to be much higher[5]) |
| Deaths | (estimated) |
Coronavirus disease 2019 (COVID-19) is a contagious disease caused by the coronavirus SARS-CoV-2. The first known case was identified in Wuhan, China, in December 2019.[7] The disease quickly spread worldwide, resulting in the COVID-19 pandemic.
The
COVID‑19 transmission occurs when infectious particles are breathed in or come into contact with the eyes, nose, or mouth. The risk is highest when people are in close proximity, but small airborne particles containing the virus can remain suspended in the air and travel over longer distances, particularly indoors. Transmission can also occur when people touch their eyes, nose or mouth after touching surfaces or objects that have been contaminated by the virus. People remain contagious for up to 20 days and can spread the virus even if they do not develop symptoms.[17]
Several COVID-19 vaccines have been approved and distributed in various countries, many of which have initiated mass vaccination campaigns. Other preventive measures include physical or social distancing, quarantining, ventilation of indoor spaces, use of face masks or coverings in public, covering coughs and sneezes, hand washing, and keeping unwashed hands away from the face. While drugs have been developed to inhibit the virus, the primary treatment is still symptomatic, managing the disease through supportive care, isolation, and experimental measures.
Nomenclature
During the initial outbreak in
Symptoms and signs
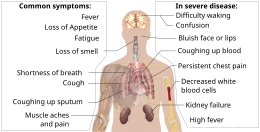
The
Published data on the neuropathological changes related with COVID-19 have been limited and contentious, with neuropathological descriptions ranging from moderate to severe
Of people who show symptoms, 81% develop only mild to moderate symptoms (up to mild
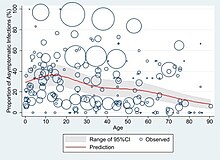
At least a third of the people who are infected with the virus do not develop noticeable symptoms at any point in time.[47][48][49] These asymptomatic carriers tend not to get tested and can still spread the disease.[49][50][51][52] Other infected people will develop symptoms later (called "pre-symptomatic") or have very mild symptoms and can also spread the virus.[52]
As is common with infections, there is a delay between the moment a person first becomes infected and the appearance of the first symptoms. The median delay for COVID-19 is four to five days[53] possibly being infectious on 1-4 of those days.[54] Most symptomatic people experience symptoms within two to seven days after exposure, and almost all will experience at least one symptom within 12 days.[53][55]
Most people recover from the acute phase of the disease. However, some people continue to experience a range of effects, such as fatigue, for months, even after recovery.[56] This is the result of a condition called long COVID, which can be described as a range of persistent symptoms that continue for weeks or months at a time.[57] Long-term damage to organs has also been observed after the onset of COVID-19. Multi-year studies are underway to further investigate the potential long-term effects of the disease.[58]
The Omicron variant became dominant in the U.S. in December 2021. Symptoms with the Omicron variant are less severe than they are with other variants.[59]Complications

Complications may include
Neurologic manifestations include
According to the US
Fungal infections such as aspergillosis, candidiasis, cryptococcosis and mucormycosis have been recorded in patients recovering from COVID‑19.[78][79]
Cause
COVID‑19 is caused by infection with a strain of coronavirus known as "severe acute respiratory syndrome coronavirus 2" (SARS-CoV-2).[80]
Transmission
COVID-19 is mainly transmitted when people breathe in air contaminated by droplets/aerosols and small airborne particles containing the virus. Infected people exhale those particles as they breathe, talk, cough, sneeze, or sing.[81][82][83][84] Transmission is more likely the closer people are. However, infection can occur over longer distances, particularly indoors.[81][85]
The transmission of the virus is carried out through virus-laden fluid particles, or droplets, which are created in the respiratory tract, and they are expelled by the mouth and the nose. There are three types of transmission: “droplet” and “contact”, which are associated with large droplets, and “airborne”, which is associated with small droplets.
Virology
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a
Outside the human body, the virus is destroyed by household soap which bursts its protective bubble.[99] Hospital disinfectants, alcohols, heat, povidone-iodine, and ultraviolet-C (UV-C) irradiation are also effective disinfection methods for surfaces.[100]
SARS-CoV-2 is closely related to the original
SARS-CoV-2 variants
The many thousands of SARS-CoV-2 variants are grouped into either clades or lineages.[106][107] The WHO, in collaboration with partners, expert networks, national authorities, institutions and researchers, have established nomenclature systems for naming and tracking SARS-CoV-2 genetic lineages by GISAID, Nextstrain and Pango. The expert group convened by the WHO recommended the labelling of variants using letters of the Greek alphabet, for example, Alpha, Beta, Delta, and Gamma, giving the justification that they "will be easier and more practical to discussed by non-scientific audiences".[108] Nextstrain divides the variants into five clades (19A, 19B, 20A, 20B, and 20C), while GISAID divides them into seven (L, O, V, S, G, GH, and GR).[109] The Pango tool groups variants into lineages, with many circulating lineages being classed under the B.1 lineage.[107][110]
Several notable variants of SARS-CoV-2 emerged throughout 2020.[111][112] Cluster 5 emerged among minks and mink farmers in Denmark.[113] After strict quarantines and a mink euthanasia campaign, the cluster was assessed to no longer be circulating among humans in Denmark as of 1 February 2021.[114]
As of December 2021[update], there are five dominant variants of SARS-CoV-2 spreading among global populations: the Alpha variant (B.1.1.7, formerly called the UK variant), first found in London and Kent, the Beta variant (B.1.351, formerly called the South Africa variant), the Gamma variant (P.1, formerly called the Brazil variant), the Delta variant (B.1.617.2, formerly called the India variant),[115] and the Omicron variant (B.1.1.529), which had spread to 57 countries as of 7 December.[116][117]
On December 19, 2023, the WHO declared that another distinctive variant, JN.1, had emerged as a "variant of interest". Though the WHO expected an increase in cases globally, particularly for countries entering winter, the overall global health risk was considered low.[118][119]
Pathophysiology

The SARS-CoV-2 virus can infect a wide range of cells and systems of the body. COVID‑19 is most known for affecting the upper respiratory tract (sinuses, nose, and throat) and the lower respiratory tract (windpipe and lungs).
Respiratory tract
Following viral entry, COVID‑19 infects the ciliated epithelium of the nasopharynx and upper airways.[123]
Autopsies of people who died of COVID‑19 have found diffuse alveolar damage, and lymphocyte-containing inflammatory infiltrates within the lung.[124]
Nervous system
One common symptom, loss of smell, results from

Research conducted when Alpha was the dominant variant has suggested COVID-19 may cause brain damage.[131] Later research showed that all variants studied (including Omicron) killed brain cells, but the exact cells killed varied by variant.[132] It is unknown if such damage is temporary or permanent.[133][134] Observed individuals infected with COVID-19 (most with mild cases) experienced an additional 0.2% to 2% of brain tissue lost in regions of the brain connected to the sense of smell compared with uninfected individuals, and the overall effect on the brain was equivalent on average to at least one extra year of normal ageing; infected individuals also scored lower on several cognitive tests. All effects were more pronounced among older ages.[135]
Gastrointestinal tract
The virus also affects gastrointestinal organs as ACE2 is abundantly expressed in the glandular cells of gastric, duodenal and rectal epithelium[136] as well as endothelial cells and enterocytes of the small intestine.[137]
Cardiovascular system
The virus can cause acute myocardial injury and chronic damage to the cardiovascular system.[138][139] An acute cardiac injury was found in 12% of infected people admitted to the hospital in Wuhan, China,[140] and is more frequent in severe disease.[141] Rates of cardiovascular symptoms are high, owing to the systemic inflammatory response and immune system disorders during disease progression, but acute myocardial injuries may also be related to ACE2 receptors in the heart.[139] ACE2 receptors are highly expressed in the heart and are involved in heart function.[139][142]
A high incidence of
COVID‑19 may also cause substantial structural changes to
Kidneys
Another common cause of death is complications related to the kidneys.[144] Early reports show that up to 30% of hospitalised patients both in China and in New York have experienced some injury to their kidneys, including some persons with no previous kidney problems.[149]
Immunopathology

Although SARS-CoV-2 has a tropism for ACE2-expressing epithelial cells of the respiratory tract, people with severe COVID‑19 have symptoms of systemic hyperinflammation. Clinical laboratory findings of elevated
Additionally, people with COVID‑19 and acute respiratory distress syndrome (ARDS) have classical serum biomarkers of CRS, including elevated C-reactive protein (CRP), lactate dehydrogenase (LDH), D-dimer, and ferritin.[153]
Systemic inflammation results in vasodilation, allowing inflammatory lymphocytic and monocytic infiltration of the lung and the heart. In particular, pathogenic GM-CSF-secreting T cells were shown to correlate with the recruitment of inflammatory IL-6-secreting monocytes and severe lung pathology in people with COVID‑19.[154] Lymphocytic infiltrates have also been reported at autopsy.[124]
Viral and host factors
Virus proteins

Multiple viral and host factors affect the pathogenesis of the virus. The S-protein, otherwise known as the spike protein, is the viral component that attaches to the host receptor via the
The M protein is the viral protein responsible for the transmembrane transport of nutrients. It is the cause of the bud release and the formation of the viral envelope.[156] The N and E protein are accessory proteins that interfere with the host's immune response.[156]
Host factors
Human
The effect of the virus on ACE2 cell surfaces leads to leukocytic infiltration, increased blood vessel permeability, alveolar wall permeability, as well as decreased secretion of lung surfactants. These effects cause the majority of the respiratory symptoms. However, the aggravation of local inflammation causes a cytokine storm eventually leading to a systemic inflammatory response syndrome.[158]
Among healthy adults not exposed to SARS-CoV-2, about 35% have
It is unknown whether different persons use similar antibody genes in response to COVID‑19.[160]
Host cytokine response

The severity of the inflammation can be attributed to the severity of what is known as the
A cytokine storm is due to an acute hyperinflammatory response that is responsible for clinical illness in an array of diseases but in COVID‑19, it is related to worse prognosis and increased fatality. The storm causes acute respiratory distress syndrome, blood clotting events such as strokes, myocardial infarction,
Pregnancy response
There are many unknowns for pregnant women during the COVID-19 pandemic. Given that they are prone to have complications and severe disease infection with other types of coronaviruses, they have been identified as a vulnerable group and advised to take supplementary preventive measures.[164]
Physiological responses to pregnancy can include:
- Immunological: The immunological response to COVID-19, like other viruses, depends on a working immune system. It adapts during pregnancy to allow the development of the foetus whose genetic load is only partially shared with their mother, leading to a different immunological reaction to infections during the course of pregnancy.[164]
- Respiratory: Many factors can make pregnant women more vulnerable to hard respiratory infections. One of them is the total reduction of the lungs' capacity and inability to clear secretions.[164]
- Coagulation: During pregnancy, there are higher levels of circulating coagulation factors, and the pathogenesis of SARS-CoV-2 infection can be implicated. The thromboembolic events with associated mortality are a risk for pregnant women.[164]
However, from the evidence base, it is difficult to conclude whether pregnant women are at increased risk of grave consequences of this virus.[164]
In addition to the above, other clinical studies have proved that SARS-CoV-2 can affect the period of pregnancy in different ways. On the one hand, there is little evidence of its impact up to 12 weeks gestation. On the other hand, COVID-19 infection may cause increased rates of unfavourable outcomes in the course of the pregnancy. Some examples of these could be foetal growth restriction, preterm birth, and perinatal mortality, which refers to the foetal death past 22 or 28 completed weeks of pregnancy as well as the death among live-born children up to seven completed days of life.[164] For preterm birth, a 2023 review indicates that there appears to be a correlation with COVID-19.[165]
Unvaccinated women in later stages of pregnancy with COVID-19 are more likely than other patients to need very intensive care. Babies born to mothers with COVID-19 are more likely to have breathing problems. Pregnant women are strongly encouraged to get vaccinated.[166]
Diagnosis
COVID‑19 can provisionally be diagnosed on the basis of symptoms and confirmed using reverse transcription polymerase chain reaction (RT-PCR) or other nucleic acid testing of infected secretions.[21][167] Along with laboratory testing, chest CT scans may be helpful to diagnose COVID‑19 in individuals with a high clinical suspicion of infection.[168] Detection of a past infection is possible with serological tests, which detect antibodies produced by the body in response to the infection.[21]
Viral testing
The standard methods of testing for presence of SARS-CoV-2 are nucleic acid tests,[21][169] which detects the presence of viral RNA fragments.[170] As these tests detect RNA but not infectious virus, its "ability to determine duration of infectivity of patients is limited".[171] The test is typically done on respiratory samples obtained by a nasopharyngeal swab; however, a nasal swab or sputum sample may also be used.[172][173] Results are generally available within hours.[21] The WHO has published several testing protocols for the disease.[174]
Several laboratories and companies have developed serological tests, which detect antibodies produced by the body in response to infection. Several have been evaluated by Public Health England and approved for use in the UK.[175]
The University of Oxford's CEBM has pointed to mounting evidence[176][177] that "a good proportion of 'new' mild cases and people re-testing positives after quarantine or discharge from hospital are not infectious, but are simply clearing harmless virus particles which their immune system has efficiently dealt with" and have called for "an international effort to standardize and periodically calibrate testing"[178] In September 2020, the UK government issued "guidance for procedures to be implemented in laboratories to provide assurance of positive SARS-CoV-2 RNA results during periods of low prevalence, when there is a reduction in the predictive value of positive test results".[179]
Imaging


Chest CT scans may be helpful to diagnose COVID‑19 in individuals with a high clinical suspicion of infection but are not recommended for routine screening.
Many groups have created
Coding
In late 2019, the WHO assigned emergency ICD-10 disease codes U07.1 for deaths from lab-confirmed SARS-CoV-2 infection and U07.2 for deaths from clinically or epidemiologically diagnosed COVID‑19 without lab-confirmed SARS-CoV-2 infection.[185]
Pathology
The main pathological findings at autopsy are:
- lung consolidation and pulmonary oedema[124]
- Lung findings:
- minor serous exudation, minor fibrin exudation[124]
- pulmonary oedema,
- exudates. DAD is the cause of acute respiratory distress syndrome (ARDS) and severe hypoxaemia.[124]
- organisation of exudates in alveolar cavities and pulmonary interstitial fibrosis[124]
- plasmocytosis in bronchoalveolar lavage (BAL)[186]
- Blood and vessels: disseminated intravascular coagulation (DIC);[187] leukoerythroblastic reaction,[188] endotheliitis,[189] hemophagocytosis[189]
- Heart: cardiac muscle cell necrosis[189]
- Liver: microvesicular steatosis[124]
- Nose: shedding of olfactory epithelium[125]
- Brain: infarction[189]
- Kidneys: acute tubular damage.[189]
- Spleen: white pulp depletion.[189]
Prevention
Preventive measures to reduce the chances of infection include getting vaccinated, staying at home, wearing a mask in public, avoiding crowded places, keeping distance from others, ventilating indoor spaces, managing potential exposure durations,[191] washing hands with soap and water often and for at least twenty seconds, practising good respiratory hygiene, and avoiding touching the eyes, nose, or mouth with unwashed hands.[192][193]
Those diagnosed with COVID‑19 or who believe they may be infected are advised by the CDC to stay home except to get medical care, call ahead before visiting a healthcare provider, wear a face mask before entering the healthcare provider's office and when in any room or vehicle with another person, cover coughs and sneezes with a tissue, regularly wash hands with soap and water and avoid sharing personal household items.[194][195]
The first
Vaccine


Prior to the
The COVID‑19 vaccines are widely credited for their role in reducing the spread of COVID‑19 and reducing the severity and death caused by COVID‑19.[204][207] According to a June 2022 study, COVID‑19 vaccines prevented an additional 14.4 to 19.8 million deaths in 185 countries and territories from 8 December 2020 to 8 December 2021.[208][209] Many countries implemented phased distribution plans that prioritized those at highest risk of complications, such as the elderly, and those at high risk of exposure and transmission, such as healthcare workers.[210][211]
Common side effects of COVID‑19 vaccines include soreness, redness, rash, inflammation at the injection site, fatigue, headache, myalgia (muscle pain), and arthralgia (joint pain), which resolve without medical treatment within a few days.[212][213] COVID‑19 vaccination is safe for people who are pregnant or are breastfeeding.[214]
As of 1 February 2024[update], 13.57 billion doses of COVID‑19 vaccines have been administered worldwide, based on official reports from national public health agencies.[215] By December 2020, more than 10 billion vaccine doses had been preordered by countries,[216] with about half of the doses purchased by high-income countries comprising 14% of the world's population.[217]Face masks and respiratory hygiene

In community and healthcare settings, the use of face masks is intended as source control to limit transmission of the virus and for personal protection to prevent infection.[218] Properly worn masks both limit the respiratory droplets and aerosols spread by infected individuals and help protect healthy individuals from infection.[219][220]
Reviews of various kinds of scientific studies have concluded that masking is effective in protecting the individual against COVID-19.[219][221][222] Various case-control and population-based studies have also shown that increased levels of masking in a community reduces the spread of SARS-CoV-2,[221][222] though there is a paucity of evidence from randomized controlled trials (RCTs).[223][224] Masks vary in how well they work, with N95 and surgical masks outperforming cloth masks,[225] but even cloth masks, with their variability in fabric type and mask fit, provide wearers with substantial protection from particles carrying COVID-19.[226]
Among readily available fabrics, double-layered cotton, hybrid masks, and cotton flannel perform best,[226] and filtration effectiveness generally improves with thread count.[225] Healthcare workers, given their exposure, are recommended against using cloth masks.[226]Indoor ventilation and avoiding crowded indoor spaces
The CDC states that avoiding crowded indoor spaces reduces the risk of COVID-19 infection.
Exhaled respiratory particles can build-up within enclosed spaces with inadequate ventilation. The risk of COVID‑19 infection increases especially in spaces where people engage in physical exertion or raise their voice (e.g., exercising, shouting, singing) as this increases exhalation of respiratory droplets. Prolonged exposure to these conditions, typically more than 15 minutes, leads to higher risk of infection.[227]
Displacement ventilation with large natural inlets can move stale air directly to the exhaust in laminar flow while significantly reducing the concentration of droplets and particles. Passive ventilation reduces energy consumption and maintenance costs but may lack controllability and heat recovery. Displacement ventilation can also be achieved mechanically with higher energy and maintenance costs. The use of large ducts and openings helps to prevent mixing in closed environments. Recirculation and mixing should be avoided because recirculation prevents dilution of harmful particles and redistributes possibly contaminated air, and mixing increases the concentration and range of infectious particles and keeps larger particles in the air.[232]
Hand-washing and hygiene

Thorough hand hygiene after any cough or sneeze is required.
Social distancing
Social distancing (also known as physical distancing) includes
In 2020, outbreaks occurred in prisons due to crowding and an inability to enforce adequate social distancing.[238][239] In the United States, the prisoner population is ageing and many of them are at high risk for poor outcomes from COVID‑19 due to high rates of coexisting heart and lung disease, and poor access to high-quality healthcare.[238]
Surface cleaning
After being expelled from the body, coronaviruses can survive on surfaces for hours to days. If a person touches the dirty surface, they may deposit the virus at the eyes, nose, or mouth where it can enter the body and cause infection.[240] Evidence indicates that contact with infected surfaces is not the main driver of COVID‑19,[241][242][243] leading to recommendations for optimised disinfection procedures to avoid issues such as the increase of antimicrobial resistance through the use of inappropriate cleaning products and processes.[244][245] Deep cleaning and other surface sanitation has been criticised as hygiene theatre, giving a false sense of security against something primarily spread through the air.[246][247]
The amount of time that the virus can survive depends significantly on the type of surface, the temperature, and the humidity.
On many surfaces, including glass, some types of plastic, stainless steel, and skin, the virus can remain infective for several days indoors at room temperature, or even about a week under ideal conditions.[248][249] On some surfaces, including cotton fabric and copper, the virus usually dies after a few hours.[248] The virus dies faster on porous surfaces than on non-porous surfaces due to capillary action within pores and faster aerosol droplet evaporation.[250][243][248] However, of the many surfaces tested, two with the longest survival times are N95 respirator masks and surgical masks, both of which are considered porous surfaces.[248]
The CDC says that in most situations, cleaning surfaces with soap or detergent, not disinfecting, is enough to reduce risk of transmission.
Self-isolation
International travel-related control measures
A 2021 Cochrane rapid review found that based upon low-certainty evidence, international travel-related control measures such as restricting cross-border travel may help to contain the spread of COVID‑19.[258] Additionally, symptom/exposure-based screening measures at borders may miss many positive cases.[258] While test-based border screening measures may be more effective, it could also miss many positive cases if only conducted upon arrival without follow-up. The review concluded that a minimum 10-day quarantine may be beneficial in preventing the spread of COVID‑19 and may be more effective if combined with an additional control measure like border screening.[258]
Treatment

The
Most cases of COVID-19 are mild. In these, supportive care includes medication such as
Although several medications have been approved in different countries as of April 2022, not all countries have these medications. Patients with mild to moderate symptoms who are in the risk groups can take
Prognosis and risk factors
The severity of COVID‑19 varies. The disease may take a mild course with few or no symptoms, resembling other common upper respiratory diseases such as the
Some early studies suggest 10% to 20% of people with COVID‑19 will experience
In terms of hospital readmissions about 9% of 106,000 individuals had to return for hospital treatment within two months of discharge. The average to readmit was eight days since first hospital visit. There are several risk factors that have been identified as being a cause of multiple admissions to a hospital facility. Among these are advanced age (above 65 years of age) and presence of a chronic condition such as diabetes, COPD, heart failure or chronic kidney disease.[298][299]
According to
It is also assumed that those that are immunocompromised are at higher risk of getting severely sick from SARS-CoV-2.[311] One research study that looked into the COVID‑19 infections in hospitalised kidney transplant recipients found a mortality rate of 11%.[312]
Men with untreated hypogonadism were 2.4 times more likely than men with eugonadism to be hospitalised if they contracted COVID-19; Hypogonad men treated with testosterone were less likely to be hospitalised for COVID-19 than men who were not treated for hypogonadism.[313]
Genetic risk factors
Children
While very young children have experienced lower rates of infection, older children have a rate of infection that is similar to the population as a whole.[320][321] Children are likely to have milder symptoms and are at lower risk of severe disease than adults.[322] The CDC reports that in the US roughly a third of hospitalised children were admitted to the ICU,[323] while a European multinational study of hospitalised children from June 2020, found that about 8% of children admitted to a hospital needed intensive care.[324] Four of the 582 children (0.7%) in the European study died, but the actual mortality rate may be "substantially lower" since milder cases that did not seek medical help were not included in the study.[325][326]
Long-term effects
Around 10% to 30% of non-hospitalised people with COVID-19 go on to develop long COVID. For those that do need hospitalisation, the incidence of long-term effects is over 50%.[15] Long COVID is an often severe multisystem disease with a large set of symptoms. There are likely various, possibly coinciding, causes.[15] Organ damage from the acute infection can explain a part of the symptoms, but long COVID is also observed in people where organ damage seems to be absent.[327]
By a variety of mechanisms, the lungs are the organs most affected in COVID‑19.
The risks of
Immunity
The
As of August 2021, reinfection with COVID‑19 was possible but uncommon. The first case of reinfection was documented in August 2020.[337] A systematic review found 17 cases of confirmed reinfection in medical literature as of May 2021.[337] With the Omicron variant, as of 2022, reinfections have become common, albeit it is unclear how common.[338] COVID-19 reinfections are thought to likely be less severe than primary infections, especially if one was previously infected by the same variant.[338][additional citation(s) needed]
Mortality
Several measures are commonly used to quantify mortality.[339] These numbers vary by region and over time and are influenced by the volume of testing, healthcare system quality, treatment options, time since the initial outbreak, and population characteristics such as age, sex, and overall health.[340]
The mortality rate reflects the number of deaths within a specific demographic group divided by the population of that demographic group. Consequently, the mortality rate reflects the prevalence as well as the severity of the disease within a given population. Mortality rates are highly correlated to age, with relatively low rates for young people and relatively high rates among the elderly.[341][342][343] In fact, one relevant factor of mortality rates is the age structure of the countries' populations. For example, the case fatality rate for COVID‑19 is lower in India than in the US since India's younger population represents a larger percentage than in the US.[344]
Case fatality rate
The case fatality rate (CFR) reflects the number of deaths divided by the number of diagnosed cases within a given time interval. Based on Johns Hopkins University statistics, the global death-to-case ratio is 1.02% (6,881,955/676,609,955) as of 10 March 2023.[345] The number varies by region.[346][347]
-
Total confirmed cases over time
-
Total confirmed cases of COVID‑19 per million people[348]
-
Total confirmed deaths over time
-
Total confirmed deaths due to COVID‑19 per million people[349]
Infection fatality rate
A key metric in gauging the severity of COVID‑19 is the
Estimates
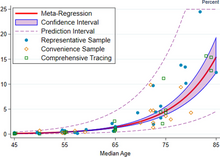

A December 2020 systematic review and meta-analysis estimated that population IFR during the first wave of the pandemic was about 0.5% to 1% in many locations (including France, Netherlands, New Zealand, and Portugal), 1% to 2% in other locations (Australia, England, Lithuania, and Spain), and exceeded 2% in Italy.[354] That study also found that most of these differences in IFR reflected corresponding differences in the age composition of the population and age-specific infection rates; in particular, the metaregression estimate of IFR is very low for children and younger adults (e.g., 0.002% at age 10 and 0.01% at age 25) but increases progressively to 0.4% at age 55, 1.4% at age 65, 4.6% at age 75, and 15% at age 85.[354] These results were also highlighted in a December 2020 report issued by the WHO.[355]
| Age group | IFR |
|---|---|
| 0–34 | 0.004% |
| 35–44 | 0.068% |
| 45–54 | 0.23% |
| 55–64 | 0.75% |
| 65–74 | 2.5% |
| 75–84 | 8.5% |
| 85 + | 28.3% |
An analysis of those IFR rates indicates that COVID‑19 is hazardous not only for the elderly but also for middle-aged adults, for whom the infection fatality rate of COVID-19 is two orders of magnitude greater than the annualised risk of a fatal automobile accident and far more dangerous than seasonal influenza.[354]
Earlier estimates of IFR
At an early stage of the pandemic, the World Health Organization reported estimates of IFR between 0.3% and 1%.[356][357] On 2 July, The WHO's chief scientist reported that the average IFR estimate presented at a two-day WHO expert forum was about 0.6%.[358][359] In August, the WHO found that studies incorporating data from broad serology testing in Europe showed IFR estimates converging at approximately 0.5–1%.[360] Firm lower limits of IFRs have been established in a number of locations such as New York City and Bergamo in Italy since the IFR cannot be less than the population fatality rate. (After sufficient time however, people can get reinfected).[361] As of 10 July, in New York City, with a population of 8.4 million, 23,377 individuals (18,758 confirmed and 4,619 probable) have died with COVID‑19 (0.3% of the population).[362] Antibody testing in New York City suggested an IFR of ≈0.9%,[363] and ≈1.4%.[364] In Bergamo province, 0.6% of the population has died.[365] In September 2020, the U.S. Centers for Disease Control and Prevention (CDC) reported preliminary estimates of age-specific IFRs for public health planning purposes.[366]
Sex differences
| Percentage of infected people who are hospitalised | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 0–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | Total | |
| Female | 0.1 (0.07–0.2) |
0.5 (0.3–0.8) |
0.9 (0.5–1.5) |
1.3 (0.7–2.1) |
2.6 (1.5–4.2) |
5.1 (2.9–8.3) |
7.8 (4.4–12.8) |
19.3 (10.9–31.6) |
2.6 (1.5–4.3) |
| Male | 0.2 (0.08–0.2) |
0.6 (0.3–0.9) |
1.2 (0.7–1.9) |
1.6 (0.9–2.6) |
3.2 (1.8–5.2) |
6.7 (3.7–10.9) |
11.0 (6.2–17.9) |
37.6 (21.1–61.3) |
3.3 (1.8–5.3) |
| Total | 0.1 (0.08–0.2) |
0.5 (0.3–0.8) |
1.1 (0.6–1.7) |
1.4 (0.8–2.3) |
2.9 (1.6–4.7) |
5.8 (3.3–9.5) |
9.3 (5.2–15.1) |
26.2 (14.8–42.7) |
2.9 (1.7–4.8) |
| Percentage of hospitalised people who go to Intensive Care Unit | |||||||||
| 0–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | Total | |
| Female | 16.7 (14.3–19.3) |
8.7 (7.5–9.9) |
11.9 (10.9–13.0) |
16.6 (15.6–17.7) |
20.7 (19.8–21.6) |
23.1 (22.2–24.0) |
18.7 (18.0–19.5) |
4.2 (4.0–4.5) |
14.3 (13.9–14.7) |
| Male | 26.9 (23.1–31.1) |
14.0 (12.2–16.0) |
19.2 (17.6–20.9) |
26.9 (25.4–28.4) |
33.4 (32.0–34.8) |
37.3 (36.0–38.6) |
30.2 (29.1–31.3) |
6.8 (6.5–7.2) |
23.1 (22.6–23.6) |
| Total | 22.2 (19.1–25.7) |
11.6 (10.1–13.2) |
15.9 (14.5–17.3) |
22.2 (21.0–23.5) |
27.6 (26.5–28.7) |
30.8 (29.8–31.8) |
24.9 (24.1–25.8) |
5.6 (5.3–5.9) |
19.0 (18.7–19.44) |
| Percent of hospitalised people who die | |||||||||
| 0–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | Total | |
| Female | 0.5 (0.2–1.0) |
0.9 (0.5–1.3) |
1.5 (1.2–1.9) |
2.6 (2.3–3.0) |
5.2 (4.8–5.6) |
10.1 (9.5–10.6) |
16.7 (16.0–17.4) |
25.2 (24.4–26.0) |
14.4 (14.0–14.8) |
| Male | 0.7 (0.3–1.5) |
1.3 (0.8–1.9) |
2.2 (1.7–2.7) |
3.8 (3.3–4.4) |
7.6 (7.0–8.2) |
14.8 (14.1–15.6) |
24.6 (23.7–25.6) |
37.1 (36.1–38.2) |
21.2 (20.8–21.7) |
| Total | 0.6 (0.2–1.3) |
1.1 (0.7–1.6) |
1.9 (1.5–2.3) |
3.3 (2.9–3.8) |
6.5 (6.0–7.0) |
12.6 (12.0–13.2) |
21.0 (20.3–21.7) |
31.6 (30.9–32.4) |
18.1 (17.8–18.4) |
| Percent of infected people who die – infection fatality rate (IFR) | |||||||||
| 0–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | Total | |
| Female | 0.001 (<0.001–0.002) |
0.004 (0.002–0.007) |
0.01 (0.007–0.02) |
0.03 (0.02–0.06) |
0.1 (0.08–0.2) |
0.5 (0.3–0.8) |
1.3 (0.7–2.1) |
4.9 (2.7–8.0) |
0.4 (0.2–0.6) |
| Male | 0.001 (<0.001–0.003) |
0.007 (0.003–0.01) |
0.03 (0.02–0.05) |
0.06 (0.03–0.1) |
0.2 (0.1–0.4) |
1.0 (0.6–1.6) |
2.7 (1.5–1.4) |
14.0 (7.9–22.7) |
0.7 (0.4–1.1) |
| Total | 0.001 (<0.001–0.002) |
0.005 (0.003–0.01) |
0.02 (0.01–0.03) |
0.05 (0.03–0.08) |
0.2 (0.1–0.3) |
0.7 (0.4–1.2) |
1.9 (1.1–3.2) |
8.3 (4.7–13.5) |
0.5 (0.3–0.9) |
| Numbers in parentheses are 95% credible intervals for the estimates. | |||||||||
COVID‑19 case fatality rates are higher among men than women in most countries. However, in a few countries like India, Nepal, Vietnam, and Slovenia the fatality cases are higher in women than men.[344] Globally, men are more likely to be admitted to the ICU and more likely to die.[368][369] One meta-analysis found that globally, men were more likely to get COVID‑19 than women; there were approximately 55 men and 45 women per 100 infections (CI: 51.43–56.58).[370]
The Chinese Center for Disease Control and Prevention reported the death rate was 2.8% for men and 1.7% for women.[371] Later reviews in June 2020 indicated that there is no significant difference in susceptibility or in CFR between genders.[372][373] One review acknowledges the different mortality rates in Chinese men, suggesting that it may be attributable to lifestyle choices such as smoking and drinking alcohol rather than genetic factors.[374] Smoking, which in some countries like China is mainly a male activity, is a habit that contributes to increasing significantly the case fatality rates among men.[344] Sex-based immunological differences, lesser prevalence of smoking in women and men developing co-morbid conditions such as hypertension at a younger age than women could have contributed to the higher mortality in men.[375] In Europe as of February 2020, 57% of the infected people were men and 72% of those died with COVID‑19 were men.[376] As of April 2020, the US government is not tracking sex-related data of COVID‑19 infections.[377] Research has shown that viral illnesses like Ebola, HIV, influenza and SARS affect men and women differently.[377]
Ethnic differences
In the US, a greater proportion of deaths due to COVID‑19 have occurred among African Americans and other minority groups.
Leaders have called for efforts to research and address the disparities.
Comorbidities
Most critical respiratory comorbidities according to the US Centers for Disease Control and Prevention (CDC), are: moderate or severe asthma, pre-existing COPD, pulmonary fibrosis, cystic fibrosis.[391] Evidence stemming from meta-analysis of several smaller research papers also suggests that smoking can be associated with worse outcomes.[392][393] When someone with existing respiratory problems is infected with COVID‑19, they might be at greater risk for severe symptoms.[394] COVID‑19 also poses a greater risk to people who misuse opioids and amphetamines, insofar as their drug use may have caused lung damage.[395]
In August 2020, the CDC issued a caution that tuberculosis (TB) infections could increase the risk of severe illness or death. The WHO recommended that people with respiratory symptoms be screened for both diseases, as testing positive for COVID‑19 could not rule out co-infections. Some projections have estimated that reduced TB detection due to the pandemic could result in 6.3 million additional TB cases and 1.4 million TB-related deaths by 2025.[396]
History
This section needs to be updated. The reason given is: excessive detail about the very early pandemic while missing an overview of the later pandemic. Please help update this article to reflect recent events or newly available information. (July 2023) |
| Part of a series on the |
| COVID-19 pandemic |
|---|
 |
|
|
International response |
|
Medical response |
|
|
|
|
The virus is thought to be of natural animal origin, most likely through
Most scientists believe the virus spilled into human populations through natural
Available evidence suggests that the SARS-CoV-2 virus was originally harboured by bats, and spread to humans multiple times from infected wild animals at the
The first confirmed human infections were in Wuhan. A study of the first 41 cases of confirmed COVID‑19, published in January 2020 in The Lancet, reported the earliest date of onset of symptoms as 1 December 2019.
By December 2019, the spread of infection was almost entirely driven by human-to-human transmission.
The Wuhan Municipal Health Commission made the first public announcement of a pneumonia outbreak of unknown cause on 31 December, confirming 27 cases[443][444][445] – enough to trigger an investigation.[446]
During the early stages of the outbreak, the number of cases doubled approximately every seven and a half days.
Italy had its first confirmed cases on 31 January 2020, two tourists from China.[452] Italy overtook China as the country with the most deaths on 19 March 2020.[453] By 26 March the United States had overtaken China and Italy with the highest number of confirmed cases in the world.[454] Research on coronavirus genomes indicates the majority of COVID-19 cases in New York came from European travellers, rather than directly from China or any other Asian country.[455] Retesting of prior samples found a person in France who had the virus on 27 December 2019,[456][457] and a person in the United States who died from the disease on 6 February 2020.[458]
RT-PCR testing of untreated wastewater samples from Brazil and Italy have suggested detection of SARS-CoV-2 as early as November and December 2019, respectively, but the methods of such sewage studies have not been optimised, many have not been peer-reviewed, details are often missing, and there is a risk of false positives due to contamination or if only one gene target is detected.[459] A September 2020 review journal article said, "The possibility that the COVID‑19 infection had already spread to Europe at the end of last year is now indicated by abundant, even if partially circumstantial, evidence", including pneumonia case numbers and radiology in France and Italy in November and December.[460]
As of 1 October 2021[update], Reuters reported that it had estimated the worldwide total number of deaths due to COVID‑19 to have exceeded five million.[461]
The Public Health Emergency of International Concern for COVID-19 ended on May 5, 2023. By this time, everyday life in most countries had returned to how it was before the pandemic.[462][463]
Misinformation
After the initial outbreak of COVID‑19, misinformation and disinformation regarding the origin, scale, prevention, treatment, and other aspects of the disease rapidly spread online.[464][465][466]
In September 2020, the US Centers for Disease Control and Prevention (CDC) published preliminary estimates of the risk of death by age groups in the United States, but those estimates were widely misreported and misunderstood.[467][468]
Other species
Humans appear to be capable of spreading the virus to some other animals,
Some pets, especially cats and
The virus does not appear to be able to infect pigs, ducks, or chickens at all.[473] Mice, rats, and rabbits, if they can be infected at all, are unlikely to be involved in spreading the virus.[475]
Tigers and lions in zoos have become infected as a result of contact with infected humans.
Research
International research on vaccines and medicines in COVID‑19 is underway by government organisations, academic groups, and industry researchers.
As of December 2020[update], hundreds of clinical trials have been undertaken, with research happening on every continent except Antarctica.[481] As of November 2020[update], more than 200 possible treatments have been studied in humans.[482]
Transmission and prevention research
Treatment-related research

Repurposed
In March 2020, the
Research on the antimalarial drugs hydroxychloroquine and chloroquine showed that they were ineffective at best,[497][498] and that they may reduce the antiviral activity of remdesivir.[499] By May 2020[update], France, Italy, and Belgium had banned the use of hydroxychloroquine as a COVID‑19 treatment.[500]
In June, initial results from the randomised RECOVERY Trial in the United Kingdom showed that dexamethasone reduced mortality by one third for people who are critically ill on ventilators and one fifth for those receiving supplemental oxygen.[501] Because this is a well-tested and widely available treatment, it was welcomed by the WHO, which is in the process of updating treatment guidelines to include dexamethasone and other steroids.[502][503] Based on those preliminary results, dexamethasone treatment has been recommended by the NIH for patients with COVID‑19 who are mechanically ventilated or who require supplemental oxygen but not in patients with COVID‑19 who do not require supplemental oxygen.[504]
In September 2020, the WHO released updated guidance on using corticosteroids for COVID‑19.[505][506] The WHO recommends systemic corticosteroids rather than no systemic corticosteroids for the treatment of people with severe and critical COVID‑19 (strong recommendation, based on moderate certainty evidence).[505] The WHO suggests not to use corticosteroids in the treatment of people with non-severe COVID‑19 (conditional recommendation, based on low certainty evidence).[505] The updated guidance was based on a meta-analysis of clinical trials of critically ill COVID‑19 patients.[507][508]
In September 2020, the
In November 2020, the US Food and Drug Administration (FDA) issued an emergency use authorisation for the investigational monoclonal antibody therapy bamlanivimab for the treatment of mild-to-moderate COVID‑19.[511] Bamlanivimab is authorised for people with positive results of direct SARS-CoV-2 viral testing who are twelve years of age and older weighing at least 40 kilograms (88 lb), and who are at high risk for progressing to severe COVID‑19 or hospitalisation.[511] This includes those who are 65 years of age or older, or who have chronic medical conditions.[511]
In February 2021, the FDA issued an emergency use authorisation (EUA) for bamlanivimab and
In April 2021, the FDA revoked the emergency use authorisation (EUA) that allowed for the investigational monoclonal antibody therapy bamlanivimab, when administered alone, to be used for the treatment of mild-to-moderate COVID‑19 in adults and certain paediatric patients.[513]
Cytokine storm

A cytokine storm can be a complication in the later stages of severe COVID‑19. A cytokine storm is a potentially deadly immune reaction where a large amount of pro-inflammatory cytokines and chemokines are released too quickly. A cytokine storm can lead to ARDS and multiple organ failure.[514] Data collected from Jin Yin-tan Hospital in Wuhan, China indicates that patients who had more severe responses to COVID‑19 had greater amounts of pro-inflammatory cytokines and chemokines in their system than patients who had milder responses. These high levels of pro-inflammatory cytokines and chemokines indicate presence of a cytokine storm.[515]
Lenzilumab, an anti-GM-CSF monoclonal antibody, is protective in murine models for CAR T cell-induced CRS and neurotoxicity and is a viable therapeutic option due to the observed increase of pathogenic GM-CSF secreting T cells in hospitalised patients with COVID‑19.[523]
Passive antibodies

Transferring purified and concentrated
The use of passive antibodies to treat people with active COVID‑19 is also being studied. This involves the production of
Bioethics
Since the outbreak of the COVID‑19 pandemic, scholars have explored the
See also
- Coronavirus diseases, a group of closely related syndromes
- Disease X, a WHO term
- Law of declining virulence– Disproved hypothesis of epidemiologist Theobald Smith
- Theory of virulence– Theory by biologist Paul W. Ewald
References
- ^ "Covid-19". Oxford English Dictionary (Online ed.). Oxford University Press. April 2020. Retrieved 15 April 2020. (Subscription or participating institution membership required.)
- ^ "Symptoms of Coronavirus". U.S. Centers for Disease Control and Prevention (CDC). 13 May 2020. Archived from the original on 17 June 2020. Retrieved 18 June 2020.
- ^ "Q&A on coronaviruses (COVID-19)". World Health Organization (WHO). 17 April 2020. Archived from the original on 14 May 2020. Retrieved 14 May 2020.
- ^ a b Ritchie H, Mathieu E, Rodés-Guirao L, Appel C, Giattino C, Ortiz-Ospina E, et al. (2020–2022). "Coronavirus Pandemic (COVID-19)". Our World in Data. Retrieved 26 April 2024.
- ^ Mathieu E, Ritchie H, Rodés-Guirao L, Appel C, Giattino C, Hasell J, et al. (5 March 2020). "Coronavirus Pandemic (COVID-19)". Our World in Data. Archived from the original on 24 February 2024. Retrieved 24 February 2024.
- ^ "The pandemic's true death toll". The Economist. 28 August 2023 [2 November 2021]. Retrieved 28 August 2023.
- ^ Page J, Hinshaw D, McKay B (26 February 2021). "In Hunt for Covid-19 Origin, Patient Zero Points to Second Wuhan Market – The man with the first confirmed infection of the new coronavirus told the WHO team that his parents had shopped there". The Wall Street Journal. Retrieved 27 February 2021.
- PMID 33822812.
- PMID 33219539.
- S2CID 229174644.
- PMID 32753137.
- PMID 36730054. Retrieved 15 November 2023.
- PMID 33481642.
- ^ "Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 6 April 2020. Archived from the original on 2 March 2020. Retrieved 19 April 2020.
- ^ PMID 36639608.
- ^ CDC (11 February 2020). "Post-COVID Conditions". U.S. Centers for Disease Control and Prevention (CDC). Retrieved 12 July 2021.
- ^ "Coronavirus disease (COVID-19): How is it transmitted?". World Health Organization (WHO). Retrieved 13 April 2023.
- ^ a b c "Overview of Testing for SARS-CoV-2, the virus that causes COVID-19". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Retrieved 31 July 2022.
- ^ a b c "Nucleic Acid Amplification Tests (NAATs)". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Retrieved 31 July 2022.
- PMID 32619959.
- ^ PMID 32621814.
- ^ "2nd U.S. Case Of Wuhan Coronavirus Confirmed". NPR. Retrieved 4 April 2020.
- from the original on 2 February 2020. Retrieved 4 April 2020.
- ^ Griffiths J. "Wuhan coronavirus deaths spike again as outbreak shows no signs of slowing". CNN. Retrieved 4 April 2020.
- PMID 32024976.
- PMID 31986261.
- S2CID 44116811.
- S2CID 214809950. Retrieved 16 April 2020.
- ^ "Novel Coronavirus (2019-nCoV) Situation Report – 1" (PDF). World Health Organization (WHO). 21 January 2020.
- ^ "Novel Coronavirus(2019-nCoV) Situation Report – 10" (PDF). World Health Organization (WHO). 30 January 2020.
- ^ "Novel coronavirus named 'Covid-19': WHO". Today. Singapore. Archived from the original on 21 March 2020. Retrieved 11 February 2020.
- ^ "The coronavirus spreads racism against – and among – ethnic Chinese". The Economist. 17 February 2020. Archived from the original on 17 February 2020. Retrieved 17 February 2020.
- hdl:10665/163636.
- ^ a b "Naming the coronavirus disease (COVID-19) and the virus that causes it". World Health Organization (WHO). Archived from the original on 28 February 2020. Retrieved 13 March 2020.
- ^ "Novel Coronavirus(2019-nCoV) Situation Report – 22" (PDF). WHO. 11 February 2020.
- PMID 32837171.
- ^ "Symptoms of Coronavirus". U.S. Centers for Disease Control and Prevention (CDC). 22 February 2021. Archived from the original on 4 March 2021. Retrieved 4 March 2021.
- S2CID 220046286.
- PMID 34192153.
- ^ "COVID toes, rashes: How the coronavirus can affect your skin". www.aad.org. Retrieved 20 March 2022.
- ^ a b "Clinical characteristics of COVID-19". European Centre for Disease Prevention and Control. 10 June 2020. Retrieved 29 December 2020.
- PMID 32600175.
- PMID 34660038.
- PMID 32483687.
- ISSN 2703-4631.
- ^ "Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 6 April 2020. Archived from the original on 2 March 2020. Retrieved 19 April 2020.
- ^ PMID 36730054.
- ^ Multiple sources:
- Oran DP, Topol EJ (May 2021). "The Proportion of SARS-CoV-2 Infections That Are Asymptomatic : A Systematic Review". Annals of Internal Medicine. 174 (5): 655–662. PMID 33481642.
- "Transmission of COVID-19". European Centre for Disease Prevention and Control. Retrieved 6 December 2020.
- Nogrady B (November 2020). "What the data say about asymptomatic COVID infections". Nature. 587 (7835): 534–535. S2CID 227079692.
- Oran DP, Topol EJ (May 2021). "The Proportion of SARS-CoV-2 Infections That Are Asymptomatic : A Systematic Review". Annals of Internal Medicine. 174 (5): 655–662.
- ^ PMID 32425996.
- PMID 32491919.
- PMID 32173241.
- ^ PMID 32364890.
- ^ PMID 32329974.
- PMID 32759252.
- S2CID 220465311.
- ^ "Half of young adults with COVID-19 had persistent symptoms after 6 months". medicalxpress.com. Retrieved 10 July 2021.
- ^ CDC (1 September 2022). "Post-COVID Conditions". Centers for Disease Control and Prevention. Retrieved 21 September 2022.
- ^ CDC (11 February 2020). "COVID-19 and Your Health". Centers for Disease Control and Prevention. Retrieved 23 January 2021.
- ^ CDC (29 March 2022). "Omicron Variant: What You Need to Know". Centers for Disease Control and Prevention. Retrieved 15 June 2022.
- PMID 31953166.
- PMID 32159735.
- PMID 32150360. Retrieved 18 March 2020.
- PMID 32061313.
- PMID 34199857.
- S2CID 227077132.
- PMID 32317203.
- PMID 32730619.
- PMID 32730555.
- PMID 32387246.
- PMID 32170806.
- ^ PMID 32282022.
- S2CID 226200547.
- PMID 32302082.
- ^ "Multisystem inflammatory syndrome in children and adolescents temporally related to COVID-19". World Health Organization (WHO). 15 May 2020. Retrieved 20 May 2020.
- ^ HAN Archive – 00432. U.S. Centers for Disease Control and Prevention (CDC) (Report). 15 May 2020. Retrieved 20 May 2020.
- PMID 32228363.
- ^ a b Córdoba-Vives S, Peñaranda G (April 2020). "COVID-19 y Embarazo". Medical Journal of Costa Rica (in Spanish): 629. Archived from the original on 18 June 2021. Retrieved 14 February 2022.
- S2CID 235782159.
- S2CID 244678882 – via ResearchGate.
- PMID 33024307.
- ^ PMID 34446582.
- PMID 33865497.
- S2CID 235823756. Retrieved 7 September 2021.
- PMID 32404416.
- PMID 32979298.
- ^ S2CID 215827809.
- S2CID 221050261.
- ^ a b c Communicable Diseases Network Australia. "Coronavirus Disease 2019 (COVID-19): CDNA National Guidelines for Public Health Units". 5.1. Communicable Diseases Network Australia/Australian Government Department of Health.
- ^ "Clinical Questions about COVID-19: Questions and Answers". Centers for Disease Control and Prevention. 4 March 2021.
- ^ "Scientific Brief: SARS-CoV-2 Transmission". Centers for Disease Control and Prevention. 7 May 2021. Retrieved 8 May 2021.
- ^ "Coronavirus disease (COVID-19): How is it transmitted?". World Health Organization. 30 April 2021.
- ^ PMID 32941052.
- ^ PMID 33853842.
- ^ S2CID 234487289. Archived from the original(PDF) on 6 December 2021. Retrieved 14 June 2021.
- S2CID 245828044.
- ^ "Outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): increased transmission beyond China – fourth update" (PDF). European Centre for Disease Prevention and Control. 14 February 2020. Retrieved 8 March 2020.
- ^ PMID 32284615.
- PMID 32015507.
- ^ Gibbens S (18 March 2020). "Why soap is preferable to bleach in the fight against coronavirus". National Geographic. Archived from the original on 2 April 2020. Retrieved 2 April 2020.
- PMID 34673114.
- PMID 31978945.
- ^ a b c Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) (PDF) (Report). World Health Organization (WHO). February 2020. Archived (PDF) from the original on 29 February 2020. Retrieved 21 March 2020.
- ^ "Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19)". World Health Organization (WHO). Retrieved 25 January 2022.
- PMID 32840560.
- PMID 33154981.
- PMID 32742035.
We detected in total 65776 variants with 5775 distinct variants.
- ^ PMID 32669681.
- ^ "Tracking SARS-CoV-2 variants". World Health Organization (WHO). 1 July 2021. Retrieved 5 July 2021.
- PMID 32794443.
- ^ "PANGO lineages". cov-lineages.org. Archived from the original on 10 May 2021. Retrieved 9 May 2021.
- S2CID 230783233.
- PMID 33761203.
- S2CID 226947606.
- PMID 33541485.
As at 1 February 2021, we assess that the cluster 5 variant is no longer circulating among humans in Denmark.
- ^ "New COVID-19 Variants". U.S. Centers for Disease Control and Prevention (CDC). 28 June 2021 [First published 11 February 2020]. Retrieved 15 July 2021.
- ^ "COVID-19 Weekly Epidemiological Update Edition 69". World Health Organization (WHO). 7 December 2021.
- ^ "Classification of Omicron (B.1.1.529): SARS-CoV-2 Variant of Concern". World Health Organization (WHO). Retrieved 9 December 2021.
- ^ "JN.1" (PDF). 19 December 2023. Retrieved 21 December 2023.
- ^ Benadjaoud Y (19 December 2023). "COVID variant JN.1 listed as 'variant of interest' by World Health Organization". ABC News. Retrieved 22 December 2023.
- PMID 33132005.
- PMID 32336612.
- PMID 32094589.
- PMID 34569339.
- ^ S2CID 221352704.
- ^ PMID 33574768.
- PMID 34078305.
- ^ PMID 32839585.
- PMID 32104915.
- PMID 32167747.
- PMID 32652139.
- PMID 35255491.
- PMID 37537664.
- ^ Geddes L, Sample I (7 March 2022). "Covid can shrink brain and damage its tissue, finds research". The Guardian. Archived from the original on 7 March 2022. Retrieved 4 September 2023.
- ^ Morelle R (7 March 2022). "Scans reveal how Covid may change the brain". BBC News. BBC. Retrieved 4 September 2023.
- ^ "Even mild Covid is linked to brain damage months after illness, scans show". NBC News. 7 March 2022.
- PMID 32142785.
- S2CID 216645754.
- PMID 35339672.
- ^ PMID 32139904.
- ^ PMID 31986264.
- ^ "Coronavirus disease 2019 (COVID-19): Myocardial infarction and other coronary artery disease issues". UpToDate. Retrieved 28 September 2020.
- PMID 15165741.
- PMID 32788101.
- ^ .
- ^ "NIH study uncovers blood vessel damage and inflammation in COVID-19 patients' brains but no infection". National Institutes of Health (NIH). 30 December 2020. Retrieved 17 January 2021.
- PMID 33378608.
- PMID 34087216.
- S2CID 220462000.
- ^ "Coronavirus: Kidney Damage Caused by COVID-19". Johns Hopkins Medicine. 14 May 2020. Retrieved 25 January 2022.
- PMID 32413319.
- PMID 33046696.
- S2CID 252566067.
- PMID 32234467.
- PMID 32801787.
- PMID 33340022.
- ^ PMID 32306836.
- PMID 32341442.
- PMID 33106832.
- PMID 32887954.
- S2CID 235786394.
- PMID 32474885.
- PMID 32707537.
- PMID 32754159.
- ^ PMID 32969772.
- PMID 36633677.
- ^ Campbell D (10 October 2021). "One in six most critically ill NHS Covid patients are unvaccinated pregnant women". The Guardian. Retrieved 25 January 2022.
- ^ PMID 32101510.
- ^ PMID 32174129.
- ^ "2019 Novel Coronavirus (2019-nCoV) Situation Summary". U.S. Centers for Disease Control and Prevention (CDC). 30 January 2020. Archived from the original on 26 January 2020. Retrieved 30 January 2020.
- ^ "Coronavirus disease (COVID-19) technical guidance: Laboratory testing for 2019-nCoV in humans". World Health Organization (WHO). Archived from the original on 15 March 2020. Retrieved 14 March 2020.
- PMID 32442256.
- ^ "Interim Guidelines for Collecting, Handling, and Testing Clinical Specimens from Persons for Coronavirus Disease 2019 (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 4 March 2020. Retrieved 26 March 2020.
- ^ "Real-Time RT-PCR Panel for Detection 2019-nCoV". U.S. Centers for Disease Control and Prevention (CDC). 29 January 2020. Archived from the original on 30 January 2020. Retrieved 1 February 2020.
- ^ "Laboratory testing for 2019 novel coronavirus (2019-nCoV) in suspected human cases". World Health Organization (WHO). Archived from the original on 17 March 2020. Retrieved 13 March 2020.
- ^ "NHS staff will be first to get new coronavirus antibody test, medical chief promises". The Independent. 14 May 2020. Retrieved 14 May 2020.
- ^ Heneghan C, Jefferson T (1 September 2020). "Virological characterization of COVID-19 patients that test re-positive for SARS-CoV-2 by RT-PCR". CEBM. Retrieved 19 September 2020.
- PMID 32853988.
- ^ Spencer E, Jefferson T, Brassey J, Heneghan C (11 September 2020). "When is Covid, Covid?". The Centre for Evidence-Based Medicine. Retrieved 19 September 2020.
- ^ "SARS-CoV-2 RNA testing: assurance of positive results during periods of low prevalence". GOV.UK. Retrieved 19 September 2020.
- ^ "ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID-19 Infection". American College of Radiology. 22 March 2020. Archived from the original on 28 March 2020.
- S2CID 222255245.
- PMID 32105641.
- ^ S2CID 212416282.
- ^ "COVID-19 Database". Società Italiana di Radiologia Medica e Interventistica (in Italian). Retrieved 11 March 2020.
- ^ "ICD-10 Version:2019". World Health Organization (WHO). 2019. Archived from the original on 31 March 2020. Retrieved 31 March 2020.
U07.2 – COVID-19, virus not identified – COVID-19 NOS – Use this code when COVID-19 is diagnosed clinically or epidemiologically but laboratory testing is inconclusive or not available. Use additional code, if desired, to identify pneumonia or other manifestations
- PMID 32194247.
- PMID 32212240.
- PMID 32212392.
- ^ S2CID 231679276.
- PMID 32269067. ("... initial exponential growth expected for an unconstrained outbreak".)
- ^ "Viral Load Exposure Factors". ReallyCorrect.com.
- ^ "Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-Based Transmission". U.S. Centers for Disease Control and Prevention (CDC). 28 June 2020.
- ^ "Scientific Brief: SARS-CoV-2 and Potential Airborne Transmission". COVID-19 Published Science and Research. U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Retrieved 30 October 2020.
- ^ Centers for Disease Control and Prevention (5 April 2020). "What to Do if You Are Sick". U.S. Centers for Disease Control and Prevention (CDC). Archived from the original on 14 February 2020. Retrieved 24 April 2020.
- ^ "Coronavirus Disease 2019 (COVID-19) – Prevention & Treatment". U.S. Centers for Disease Control and Prevention (CDC). 10 March 2020. Archived from the original on 11 March 2020. Retrieved 11 March 2020.
- ^ "UK medicines regulator gives approval for first UK COVID-19 vaccine". Medicines and Healthcare Products Regulatory Agency, Government of the UK. 2 December 2020. Retrieved 2 December 2020.
- ^ Mueller B (2 December 2020). "U.K. Approves Pfizer Coronavirus Vaccine, a First in the West". The New York Times. Archived from the original on 2 December 2020. Retrieved 2 December 2020.
- ^ "COVID-19 Treatment Guidelines". nih.gov. National Institutes of Health. Retrieved 21 April 2020.
- ^ PMID 32164834.
A key issue for epidemiologists is helping policy makers decide the main objectives of mitigation – e.g. minimising morbidity and associated mortality, avoiding an epidemic peak that overwhelms health-care services, keeping the effects on the economy within manageable levels, and flattening the epidemic curve to wait for vaccine development and manufacture on scale and antiviral drug therapies.
- ^ Wiles S (14 March 2020). "After 'Flatten the Curve', we must now 'Stop the Spread'. Here's what that means". The Spinoff. Archived from the original on 26 March 2020. Retrieved 13 March 2020.
- ^ "Data on COVID-19 mortality by vaccination status". Our World in Data (CDC data). April 2023. Archived from the original on 16 October 2023.
Data source: Centers for Disease Control and Prevention, Vaccine Breakthrough/Surveillance and Analytics Team.
- PMID 33341119.
- PMID 34265245.
- ^ a b c d Rogers K (11 May 2022). "COVID-19 vaccine". Encyclopædia Britannica. Archived from the original on 12 June 2022. Retrieved 12 June 2022.
- ^ "Swissmedic grants authorisation for the first COVID-19 vaccine in Switzerland" (Press release). Swiss Agency for Therapeutic Products (Swissmedic). 18 December 2020. Archived from the original on 2 May 2021. Retrieved 5 July 2022.
- ^ "EMA recommends first COVID-19 vaccine for authorisation in the EU". European Medicines Agency (EMA) (Press release). 21 December 2020. Archived from the original on 30 January 2021. Retrieved 21 December 2020.
- S2CID 245262732.
- PMID 35753318.
- ^ "COVID-19 vaccines saved nearly 20 million lives in a year, study says". CBS News. 24 June 2022. Archived from the original on 29 June 2022. Retrieved 27 June 2022.
- from the original on 18 January 2021. Retrieved 26 December 2020.
- S2CID 236515442.
- hdl:10665/339218. WHO/2019-nCoV/vaccines/SAGE_recommendation/mRNA-1273/background/2021.1. Archivedfrom the original on 13 June 2021. Retrieved 24 July 2021.
- ^ "Background document on the mRNA-1273 vaccine (Moderna) against COVID-19". World Health Organization (WHO). Archived from the original on 26 January 2022. Retrieved 23 January 2022.
- ^ "Pregnancy, breastfeeding, fertility and coronavirus (COVID-19) vaccination". NHS. 5 October 2022. Archived from the original on 15 October 2022. Retrieved 15 October 2022.
- ^ Richie H, Ortiz-Ospina E, Beltekian D, Methieu E, Hasell J, Macdonald B, et al. (March 2020). "Coronavirus (COVID-19) Vaccinations – Statistics and Research". Our World in Data. Archived from the original on 10 March 2021. Retrieved 7 February 2021.
- S2CID 227246811.
- PMID 33323376.
- S2CID 235823756.
- ^ PMID 32787926.
- S2CID 236947786.
Masks prevent the spread of droplets and aerosols generated by an infected individual, and when correctly worn surgical masks can reduce viral transmission by 95%. Uninfected individuals wearing a surgical mask are about 85% protected against infection.
- ^ S2CID 244271780.
The results of additional studies that assessed mask wearing ... indicate a reduction in covid-19 incidence, SARS-CoV-2 transmission, and covid-19 mortality. Specifically, a natural experiment across 200 countries showed 45.7% fewer covid-19 related mortality in countries where mask-wearing was mandatory. Another natural experiment study in the US reported a 29% reduction in SARS-CoV-2 transmission (measured as the time-varying reproductive number Rt) (risk ratio 0.71, 95% confidence interval 0.58 to 0.75) in states where mask-wearing was mandatory. A comparative study in the Hong Kong Special Administrative Region reported a statistically significantly lower cumulative incidence of covid-19 associated with mask-wearing than in selected countries where mask-wearing was not mandatory.
- ^ a b "Science Brief: Community Use of Masks to Control the Spread of SARS-CoV-2". CDC. 11 February 2020.
Experimental and epidemiologic data support community masking to reduce the spread of SARS-CoV-2, including alpha and delta variants, among adults and children. [...] Mask use has been found to be safe and is not associated with clinically significant impacts on respiration or gas exchange under most circumstances, except for intense exercise. The limited available data indicate no clear evidence that masking impairs emotional or language development in children. [I]n combination with other contextual cues, masks are unlikely to produce serious impairments of children's social interactions. A study of 2-year-old children concluded that they were able to recognize familiar words presented without a mask and when hearing words through opaque masks. Among children with autism spectrum disorders (ASD), interventions including positive reinforcement and coaching caregivers to teach mask-wearing have improved participants' ability to wear a face mask. These findings suggest that even children who may have difficulty wearing a mask can do so effectively through targeted interventions.
- PMID 36715243.
- PMID 37611625.
- ^ PMID 33971389.
- ^ PMID 34689269.
- ^ a b c CDC (11 February 2020). "Scientific Brief: SARS-CoV-2 Transmission". U.S. Centers for Disease Control and Prevention (CDC). Retrieved 10 May 2021.
- ^ "Transmission of COVID-19". European Centre for Disease Prevention and Control. 7 September 2020. Retrieved 14 October 2020.
- ^ a b National Center for Immunization and Respiratory Diseases (NCIRD) (9 July 2020). "COVID-19 Employer Information for Office Buildings". U.S. Centers for Disease Control and Prevention (CDC). Retrieved 9 July 2020.
- .
- PMID 32473123.
- S2CID 221642242.
- ^ "Social distancing: what you need to do – Coronavirus (COVID-19)". nhs.uk. 2 June 2020. Retrieved 18 August 2020.
- ^ "Advice for the public on COVID-19 – World Health Organization". World Health Organization (WHO). Retrieved 18 August 2020.
- ^ "COVID-19 and Your Health". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Retrieved 23 March 2021.
To prevent the spread of germs, including COVID-19, CDC recommends washing hands with soap and water whenever possible because it reduces the amount of many types of germs and chemicals on hands. But if soap and water are not readily available, using a hand sanitizer with at least 60% alcohol can help you avoid getting sick and spreading germs to others.
- ^ "WHO-recommended handrub formulations". WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care. World Health Organization (WHO). 19 March 2009. Retrieved 19 March 2020.
- PMID 33959956.
- ^ PMID 32343355.
- ^ Waldstein D (6 May 2020). "To Fight Virus in Prisons, C.D.C. Suggests More Screenings". The New York Times. Archived from the original on 7 May 2020. Retrieved 14 May 2020.
- ^ "How COVID-19 Spreads". U.S. Centers for Disease Control and Prevention (CDC). 18 September 2020. Archived from the original on 19 September 2020. Retrieved 20 September 2020.
- PMID 32628907.
- ^ Weixel N (5 April 2021). "CDC says risk of COVID-19 transmission on surfaces 1 in 10,000". The Hill. Retrieved 19 December 2021.
- ^ a b "Science Brief: SARS-CoV-2 and Surface (Fomite) Transmission for Indoor Community Environments". U.S. Centers for Disease Control and Prevention (CDC). 5 April 2021. Archived from the original on 5 April 2021.
- ^ S2CID 231900820.
- PMID 33384670.
- ^ Thompson D (8 February 2021). "Hygiene Theater Is Still a Huge Waste of Time". The Atlantic. Retrieved 27 February 2021.
- ^ Thompson D (27 July 2020). "Hygiene Theater Is a Huge Waste of Time". The Atlantic. Retrieved 27 February 2021.
- ^ PMID 33218120.
- PMID 33281435.
- PMID 33746485.
- ^ CDC (11 February 2020). "Coronavirus Disease 2019 (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). Retrieved 12 April 2021.
- ^ Anthes E (8 April 2021). "Has the Era of Overzealous Cleaning Finally Come to an End?". The New York Times. Archived from the original on 28 December 2021. Retrieved 12 April 2021.
- ^ "Interim Recommendations for US Community Facilities with Suspected/Confirmed Coronavirus Disease 2019". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Retrieved 4 April 2020.
- ^ "Yes, UV phone sanitizers work. That doesn't mean you need one". The Washington Post. 16 February 2021. Retrieved 29 April 2022.
- PMID 33012884.
- ^ "COVID-19 Informational Resources for High-Risk Groups | Keeping Education ACTIVE | Partnership to Fight Chronic Disease". fightchronicdisease.org. Retrieved 31 May 2020.
- ^ "Quarantine and Isolation". U.S. Centers for Disease Control and Prevention (CDC). 29 July 2021. Retrieved 12 August 2021.
- ^ S2CID 232356197.
- PMID 32106852.
- PMID 32044814.
- PMID 32171074.
- S2CID 236472654.
- ^ a b Motseki TP (7 June 2022). "COVID-19 Vaccination Guidelines". www.nih.gov. National Institutes of Health. Archived from the original on 19 January 2021. Retrieved 18 January 2021.
- PMID 32134116.
- ^ "Coronavirus". WebMD. Archived from the original on 1 February 2020. Retrieved 1 February 2020.
- PMID 32387333.
- ^ "Coronavirus recovery: breathing exercises". www.hopkinsmedicine.org. Johns Hopkins Medicine. Archived from the original on 11 October 2020. Retrieved 30 July 2020.
- PMID 32201353.
- ^ U.S. Centers for Disease Control and Prevention (5 April 2020). "What to Do if You Are Sick". U.S. Centers for Disease Control and Prevention (CDC). Archived from the original on 14 February 2020. Retrieved 24 April 2020.
- S2CID 227059995.
- ^ "Q&A: Dexamethasone and COVID-19". World Health Organization (WHO). Archived from the original on 11 October 2020. Retrieved 11 July 2020.
- National COVID-19 Clinical Evidence Taskforce. Archivedfrom the original on 11 October 2020. Retrieved 11 July 2020.
- PMID 32109013.
- PMID 32178774.
- PMID 33391477.
- ^ "COVID Treatment Guidelines: Clinical Management Summary". NIH Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. 8 April 2022. Archived from the original on 5 November 2021. Retrieved 19 April 2022.
- ^ Wise J (17 April 2022). "What Happened to Paxlovid, the COVID Wonder Drug?". Intelligencer. Archived from the original on 19 April 2022. Retrieved 19 April 2022.
- PMID 33849936.
- ^ Aripaka P (5 November 2021). "Britain approves Merck's COVID-19 pill in world first". Reuters. Archived from the original on 8 November 2021. Retrieved 8 November 2021.
- ^ Beasley D (5 November 2021). "Pfizer says its antiviral pill slashes risk of severe COVID-19 by 89%". Reuters. Archived from the original on 7 November 2021. Retrieved 8 November 2021.
- PMID 38032024.
- ^ PMID 32732190.
- ^ PMID 33175121.
- ^ a b c "COVID-19 Treatment Guidelines". www.nih.gov. National Institutes of Health. Archived from the original on 19 January 2021. Retrieved 18 January 2021./
- ^ Saima MS (2 November 2021). "Common Antidepressant Slashes Risk of COVID Death". Nature. Archived from the original on 8 November 2021. Retrieved 8 November 2021.
- PMID 33214186.
- ^ Reed J (4 November 2021). "Molnupiravir: First pill to treat Covid gets approval in UK". www.bbc.co.uk. Archived from the original on 4 November 2021. Retrieved 23 November 2021.
- S2CID 224817161.
- ^ a b Palmieri L, Andrianou X, Barbariol P, Bella A, Bellino S, Benelli E, et al. (22 July 2020). Characteristics of SARS-CoV-2 patients dying in Italy Report based on available data on July 22nd, 2020 (PDF) (Report). Istituto Superiore di Sanità. Retrieved 4 October 2020.
- PMID 33624101.
- PMID 34370712.
- S2CID 227065216.
- PMID 32877961.
- .
- ^ "How long does COVID-19 last?". UK COVID Symptom Study. 6 June 2020. Retrieved 15 October 2020.
- ^ "Summary of COVID-19 Long Term Health Effects: Emerging evidence and Ongoing Investigation" (PDF). University of Washington. 1 September 2020. Archived from the original (PDF) on 18 December 2020. Retrieved 15 October 2020.
- ^ "Long-term symptoms of COVID-19 'really concerning', says WHO chief". UN News. 30 October 2020. Retrieved 7 March 2021.
- ^ "Coronavirus disease 2019 (COVID-19) – Prognosis". BMJ. Retrieved 15 November 2020.
- PMID 33180754.
- PMID 32206052.
- ^ PMID 32422280.
- PMID 32973066.
- PMID 33148655.
- .
- PMID 32580440.
- PMID 32718835.
- ^ "COVID-19: Who's at higher risk of serious symptoms?". Mayo Clinic.
- PMID 32438328.
- PMID 32377709.
- PMID 33855033.
- ^ "Coronavirus Disease 2019 (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020.
- PMID 32775986.
- PMID 36053534.
- S2CID 233372385.
- ^ Wallis C. "One in Seven Dire COVID Cases May Result from a Faulty Immune Response". Scientific American.
- S2CID 221914095.
- PMID 23462180.
- PMID 35940203.
- PMID 35255492.
- ^ "COVID-19 in children and the role of school settings in transmission – first update". European Centre for Disease Prevention and Control. 23 December 2020. Retrieved 6 April 2021.
- ^ "Estimated Disease Burden of COVID-19". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Retrieved 6 April 2021.
- S2CID 239653475. Retrieved 7 September 2021.
- ^ "Information for Pediatric Healthcare Providers". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Retrieved 6 April 2021.
- PMID 32593339.
- PMID 32171062.
- ^ "Coronavirus Disease 2019 (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 2 March 2020. Retrieved 2 March 2020.
- PMID 35594336.
- ^ S2CID 227162748.
- PMID 33006087.
- PMID 32838236.
- ^ "COVID-19 Lung Damage". Johns Hopkins Medicine. 28 February 2022. Retrieved 21 May 2022.
- S2CID 251626731.
- ^ "Immune responses and correlates of protective immunity against SARS-CoV-2". European Centre for Disease Prevention and Control. 18 May 2021. Retrieved 3 June 2021.
- PMID 32505227.
- PMID 34126625.
- ^ S2CID 229323810.
- ^ S2CID 234773697.
- ^ a b "How soon after catching COVID-19 can you get it again?". ABC News. 2 May 2022. Retrieved 24 June 2022.
- ^ Centers for Disease Control and Prevention (May 2012). "Lesson 3: Measures of Risk Section 3: Mortality Frequency Measures". Principles of Epidemiology in Public Health Practice (Third ed.). U.S. Centers for Disease Control and Prevention (CDC). No. SS1978. Archived from the original on 28 February 2020. Retrieved 28 March 2020.
- ^ Ritchie H, Roser M (25 March 2020). Chivers T (ed.). "What do we know about the risk of dying from COVID-19?". Our World in Data. Archived from the original on 28 March 2020. Retrieved 28 March 2020.
- PMID 32320004.
- PMID 32187458.
- S2CID 219118986.
- ^ PMID 33160453.
- ^ "COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU)". ArcGIS. Johns Hopkins University. Retrieved 10 March 2023.
- PMID 32199072.
- ^ Ritchie H, Ortiz-Ospina E, Beltekian D, Mathieu E, Hasell J, MacDonald B, et al. (5 March 2020). "What do we know about the risk of dying from COVID-19?". Our World in Data. Archived from the original on 28 March 2020. Retrieved 28 March 2020.
- ^ "Total confirmed cases of COVID-19 per million people". Our World in Data. Archived from the original on 19 March 2020. Retrieved 21 June 2022.[needs update]
- ^ "Cumulative confirmed COVID-19 deaths per million people". Our World in Data.
- S2CID 219726496.
- PMID 33069277.
- PMID 33007452.
- PMID 32837360.
- ^ PMID 33289900..
 Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License Archived 16 October 2017 at the Wayback Machine
Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License Archived 16 October 2017 at the Wayback Machine - hdl:10665/338095.
- ^ "Coronavirus disease 2019 (COVID-19) Situation Report – 30" (PDF). 19 February 2020. Retrieved 3 June 2020.
- ^ "Coronavirus disease 2019 (COVID-19) Situation Report – 31" (PDF). 20 February 2020. Retrieved 23 April 2020.
- ^ McNeil Jr DG (4 July 2020). "The Pandemic's Big Mystery: How Deadly Is the Coronavirus? – Even with more than 500,000 dead worldwide, scientists are struggling to learn how often the virus kills. Here's why". The New York Times. Archived from the original on 4 July 2020. Retrieved 6 July 2020.
- ^ "Global Research and Innovation Forum on COVID-19: Virtual Press Conference" (PDF). World Health Organization (WHO). 2 July 2020.
- ^ "Estimating mortality from COVID-19". World Health Organization (WHO). Retrieved 21 September 2020.
- PMID 34720322.
- ^ "COVID-19: Data". City of New York.
- SSRN 3590771.
- PMID 33091374.
- ^ Modi C (21 April 2020). "How deadly is COVID-19? Data Science offers answers from Italy mortality data". Medium. Retrieved 23 April 2020.
- ^ "Coronavirus Disease 2019 (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 10 September 2020. Retrieved 9 December 2020.
- PMID 32404476.
- ^ McIntosh K (April 2021). "Covid 19 Clinical Features". UpToDate. Retrieved 12 May 2021.
- PMID 33298944.
- PMID 33028563.
- ^ PMID 34594836.
- PMID 32315817.
- PMID 32283155.
- S2CID 216028003.
- ^ Rabin RC (20 March 2020). "In Italy, Coronavirus Takes a Higher Toll on Men". The New York Times. Archived from the original on 20 March 2020. Retrieved 7 April 2020.
- ^ "COVID-19 weekly surveillance report". World Health Organization (WHO). Archived from the original on 15 March 2020. Retrieved 7 April 2020.
- ^ a b Gupta AH (3 April 2020). "Does Covid-19 Hit Women and Men Differently? U.S. Isn't Keeping Track". The New York Times. Archived from the original on 3 April 2020. Retrieved 7 April 2020.
- ^ PMID 32305087.
- ^ PMID 34293038.
- PMID 32324118.
- ^ Batthyány K (13 October 2020). "Coronavirus y Desigualdades preexistentes: Género y Cuidados". CLACSO (Consejo Latinoamericano de Ciencias Sociales). Retrieved 22 April 2021.
- ^ "COVID-19 Presents Significant Risks for American Indian and Alaska Native People". 14 May 2020.
- ^ "COVID-19 Presents Significant Risks for American Indian and Alaska Native People". 14 May 2020.
- PMID 32306369.
- ^ "How coronavirus deaths in the UK compare by race and ethnicity". The Independent. 9 June 2020. Retrieved 10 June 2020.
- ^ "Emerging findings on the impact of COVID-19 on black and minority ethnic people". The Health Foundation. Retrieved 10 June 2020.
- ^ Butcher B, Massey J (9 June 2020). "Why are more BAME people dying from coronavirus?". BBC News. Retrieved 10 June 2020.
- ^ a b c "The ancient Neanderthal hand in severe COVID-19". ScienceDaily. 30 September 2020. Retrieved 13 December 2020.
- ^ "WHO Director-General's statement on the advice of the IHR Emergency Committee on Novel Coronavirus". World Health Organization (WHO).
- PMID 32298251.
- ^ "Coronavirus Disease 2019 (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Retrieved 19 June 2020.
- PMID 32293753.
- ^ "Smoking and COVID-19". World Health Organization (WHO). Retrieved 19 June 2020.
- ^ "Coronavirus Disease 2019 (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Retrieved 4 May 2020.
- ^ DeRobertis J (3 May 2020). "People who use drugs are more vulnerable to coronavirus. Here's what clinics are doing to help". The Advocate (Louisiana). Retrieved 4 May 2020.
- ^ "Coronavirus Disease 2019 (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020.
- PMID 33744401.
- PMID 34480864.
- ^ "WHO-convened Global Study of Origins of SARS-CoV-2: China Part". World Health Organization (WHO). 30 March 2021. Retrieved 29 July 2022.
- ^ Duarte F (24 February 2020). "As the cases of coronavirus increase in China and around the world, the hunt is on to identify "patient zero"". BBC News. Retrieved 22 March 2020.
- PMID 35881005.
- ^ Gill V (26 July 2022). "Covid origin studies say evidence points to Wuhan market". BBC News Online. BBC. Archived from the original on 26 July 2022. Retrieved 31 August 2023.
- S2CID 251067542.
- ^ "Debate deepens over Wuhan wet market's role in kickstarting the pandemic". National Geographic. 27 July 2022.
- PMID 32104911.
- PMID 32284615.
- PMID 32387564.
- ^ Grose TK (13 May 2020). "Did the Coronavirus Originate Outside of Wuhan?". U.S. News & World Report.
- ^ PMID 35881005.
- ^ S2CID 251843410. Retrieved 20 November 2022.
- ^ Terrestrial and Freshwater Ecosystems and Their Services. In: Climate Change 2022: Impacts, Adaptation and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change (PDF). IPCC. 2022. pp. 233–235. Retrieved 14 March 2023.
- ^ Health, Wellbeing, and the Changing Structure of Communities. In: Climate Change 2022: Impacts, Adaptation and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change (PDF). IPCC. 2022. pp. 1067–1070. Retrieved 14 March 2023.
- ^ "Climate change may have driven the emergence of SARS-CoV-2". University of Cambridge. Science of the Total Environment. 5 February 2021. Retrieved 14 March 2023.
- ^ "Climate change the culprit in the COVID-19 pandemic". European Commission. Retrieved 24 March 2023.
- ^ Barnes JE (26 February 2023). "Lab Leak Most Likely Caused Pandemic, Energy Dept. Says". The New York Times. Retrieved 27 February 2023.
- ^ Mueller J (26 February 2023). "Energy Department's COVID lab leak conclusion: What we know". The Hill. Retrieved 26 March 2023.
- ^ LeBlanc P (27 February 2023). "New assessment on the origins of Covid-19 adds to the confusion | CNN Politics". CNN. Retrieved 27 February 2023.
- ^ Davis N, Hawkins A (27 February 2023). "How seriously should we take the US DoE's Covid lab leak theory?". The Guardian. Retrieved 27 February 2023.
- ^ Wolf ZB (25 May 2021). "Analysis: Why scientists are suddenly more interested in the lab-leak theory of Covid's origin". CNN. Retrieved 26 May 2021.
- S2CID 237373547.
- ^ Paun C, Zeller S, Reader R, Leonard B, Scullion G (4 November 2022). "Cross-examining the lab-leak theorists". Politico. Retrieved 21 November 2022.
- ^ Hosenball M, Zengerle P (30 October 2021). "U.S. spy agencies say origins of COVID-19 may never be known". Reuters. Retrieved 21 November 2022.
- PMID 34480864.
Under any laboratory escape scenario, SARS-CoV-2 would have to have been present in a laboratory prior to the pandemic, yet no evidence exists to support such a notion and no sequence has been identified that could have served as a precursor.
- ^ Gorski D (31 May 2021). "The origin of SARS-CoV-2, revisited". Science-Based Medicine. Archived from the original on 1 June 2021. Retrieved 19 July 2021.
The second [version of the lab leak] is the version that "reasonable" people consider plausible, but there is no good evidence for either version.
- ^ Holmes EC (14 August 2022). "The COVID lab leak theory is dead. Here's how we know the virus came from a Wuhan market". The Conversation. Retrieved 4 September 2022.
For the lab leak theory to be true, SARS-CoV-2 must have been present in the Wuhan Institute of Virology before the pandemic started. This would convince me. But the inconvenient truth is there's not a single piece of data suggesting this. There's no evidence for a genome sequence or isolate of a precursor virus at the Wuhan Institute of Virology. Not from gene sequence databases, scientific publications, annual reports, student theses, social media, or emails. Even the intelligence community has found nothing. Nothing. And there was no reason to keep any work on a SARS-CoV-2 ancestor secret before the pandemic.
- PMID 32134861.
- PMID 31986257.
- .
- ^ "Novel Coronavirus – China". World Health Organization (WHO). 12 January 2020. Archived from the original on 14 January 2020.
- ^ Kessler G (17 April 2020). "Trump's false claim that the WHO said the coronavirus was 'not communicable'". The Washington Post. Archived from the original on 17 April 2020. Retrieved 17 April 2020.
- ^ Kuo L (21 January 2020). "China confirms human-to-human transmission of coronavirus". The Guardian. Retrieved 18 April 2020.
- S2CID 211133882.
- ^ Areddy JT (26 May 2020). "China Rules Out Animal Market and Lab as Coronavirus Origin". The Wall Street Journal. Retrieved 29 May 2020.
- ^ Kelland K (19 June 2020). "Italy sewage study suggests COVID-19 was there in December 2019". Reuters. Retrieved 23 June 2020.
- PMID 32061313.
- ^ Bryner J (14 March 2020). "1st known case of coronavirus traced back to November in China". livescience.com. Retrieved 31 May 2020.
- ^ Canadian Politics (8 April 2020). "The birth of a pandemic: How COVID-19 went from Wuhan to Toronto". National Post. Retrieved 31 May 2020.
- ^ 高昱 (26 February 2020). "独家 | 新冠病毒基因测序溯源: 警报是何时拉响的" [Exclusive | Tracing the New Coronavirus gene sequencing: when did the alarm sound]. Caixin (in Chinese). Archived from the original on 27 February 2020. Retrieved 1 March 2020.
- ^ 路子康. "最早上报疫情的她, 怎样发现这种不一样的肺炎". 中国网新闻 (in Chinese (China)). 北京. Archived from the original on 2 March 2020. Retrieved 11 February 2020.
- ^ "Undiagnosed pneumonia – China (HU): RFI". ProMED Mail. ProMED. Retrieved 7 May 2020.
- ^ "'Hero who told the truth': Chinese rage over coronavirus death of whistleblower doctor". The Guardian. 7 February 2020.
- ^ Kuo L (11 March 2020). "Coronavirus: Wuhan doctor speaks out against authorities". The Guardian. London.
- ^ "Novel Coronavirus". World Health Organization (WHO). Archived from the original on 2 February 2020. Retrieved 6 February 2020.
- ^ "武汉现不明原因肺炎 官方确认属实: 已经做好隔离". Xinhua Net 新華網. 31 December 2019. Retrieved 31 March 2020.
- ^ 武汉市卫健委关于当前我市肺炎疫情的情况通报. WJW.Wuhan.gov.cn (in Chinese). Wuhan Municipal Health Commission. 31 December 2019. Archived from the original on 9 January 2020. Retrieved 8 February 2020.
- ^ "Mystery pneumonia virus probed in China". BBC News. 3 January 2020. Archived from the original on 5 January 2020. Retrieved 29 January 2020.
- PMID 31995857.
- ^ "China confirms sharp rise in cases of SARS-like virus across the country". 20 January 2020. Archived from the original on 20 January 2020. Retrieved 20 January 2020.
- ^ a b "Flattery and foot dragging: China's influence over the WHO under scrutiny". The Globe and Mail. 25 April 2020.
- ^ Horton R (18 March 2020). "Scientists have been sounding the alarm on coronavirus for months. Why did Britain fail to act?". The Guardian. Retrieved 23 April 2020.
- ^ "China delayed releasing coronavirus info, frustrating WHO". Associated Press. 2 June 2020. Retrieved 3 June 2020.
- ^ "Coronavirus: Primi due casi in Italia" [Coronavirus: First two cases in Italy]. Corriere della sera (in Italian). 31 January 2020. Retrieved 31 January 2020.
- ^ "Coronavirus: Number of COVID-19 deaths in Italy surpasses China as total reaches 3,405". Sky News. Retrieved 7 May 2020.
- McNeil Jr DG (26 March 2020). "The U.S. Now Leads the World in Confirmed Coronavirus Cases". The New York Times. Archivedfrom the original on 26 March 2020. Retrieved 27 March 2020.
- ^ "Studies Show N.Y. Outbreak Originated in Europe". The New York Times. 8 April 2020. Archived from the original on 8 April 2020.
- ^ Irish J (4 May 2020). Lough RM, Graff P (eds.). "After retesting samples, French hospital discovers COVID-19 case from December". Reuters. Retrieved 4 May 2020.
- PMID 32371096.
- ^ "2 died with coronavirus weeks before 1st U.S. virus death". PBS NewsHour. 22 April 2020. Retrieved 23 April 2020.
- PMID 32834990.
- PMID 32973152.
- ^ Kavya B, Abraham R (3 October 2021). Shumaker L, Wardell J (eds.). "Global COVID-19 deaths hit 5 million as Delta variant sweeps the world". Reuters.com. Reuters.
- ^ "From emergency response to long-term COVID-19 disease management: sustaining gains made during the COVID-19 pandemic". World Health Organization (WHO). Retrieved 9 May 2023.
- ^ Heyward G, Silver M (5 May 2023). "WHO ends global health emergency declaration for COVID-19". NPR. Retrieved 9 May 2023.
- ^ "China coronavirus: Misinformation spreads online about origin and scale". BBC News. 30 January 2020. Archived from the original on 4 February 2020. Retrieved 10 February 2020.
- ^ Taylor J (31 January 2020). "Bat soup, dodgy cures and 'diseasology': the spread of coronavirus misinformation". The Guardian. Archived from the original on 2 February 2020. Retrieved 3 February 2020.
- ^ "Here's A Running List Of Disinformation Spreading About The Coronavirus". Buzzfeed News. Archived from the original on 6 February 2020. Retrieved 8 February 2020.
- ^ "Coronavirus Disease 2019 (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Retrieved 10 October 2020.
- ^ "Misleading claim circulates online about infection fatality ratio of Covid-19 in the US". Fact Check. 8 October 2020. Retrieved 10 October 2020.
- PMID 33230363.
- PMID 35624123. Retrieved 28 February 2023.
- PMID 36363758.
- PMID 32967592.
- ^ PMID 32956786.
- PMID 32269068.
- ^ PMID 32957995.
- ^ from the original on 28 December 2021. Retrieved 24 February 2021.
- PMID 32186952.
- PMID 32052466.
- ^ "Interim Laboratory Biosafety Guidelines for Handling and Processing Specimens Associated with Coronavirus Disease 2019 (COVID-19)". Coronavirus Disease 2019 (COVID-19) Lab Biosafety Guidelines. U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Retrieved 1 April 2020.
- .
- . Retrieved 8 March 2022.
- ^ Reardon S (November 2020). "For COVID Drugs, Months of Frantic Development Lead to Few Outright Successes". Scientific American. Retrieved 10 December 2020.
- PMID 32171059.
- S2CID 231775762.
- PMID 32322102.
- PMID 32220655.
- PMID 32202722.
- .
- .
- PMID 32834509.
- PMID 32621869.
- S2CID 216307705.
- ^ "COVID-19 treatment and vaccine tracker" (PDF). Milken Institute. 21 April 2020. Retrieved 21 April 2020.
- ^ a b Koch S, Pong W (13 March 2020). "First up for COVID-19: nearly 30 clinical readouts before end of April". BioCentury Inc. Retrieved 1 April 2020.
- .
- ^ "UN health chief announces global 'solidarity trial' to jumpstart search for COVID-19 treatment". UN News. 18 March 2020. Archived from the original on 23 March 2020. Retrieved 23 March 2020.
- ^ "Citing safety concerns, the W.H.O. paused tests of a drug Trump said he had taken". The New York Times. 26 May 2020. Archived from the original on 26 May 2020.
- ^
 This article incorporates text from this source, which is in the public domain: Hydroxychloroquine does not benefit adults hospitalized with COVID-19. National Institutes of Health (NIH). 9 November 2020. Retrieved 9 November 2020.
This article incorporates text from this source, which is in the public domain: Hydroxychloroquine does not benefit adults hospitalized with COVID-19. National Institutes of Health (NIH). 9 November 2020. Retrieved 9 November 2020.
- ^
 This article incorporates text from this source, which is in the public domain: Coronavirus (COVID-19) Update: FDA Warns of Newly Discovered Potential Drug Interaction That May Reduce Effectiveness of a COVID-19 Treatment Authorized for Emergency Use. U.S. Food and Drug Administration (FDA). 15 June 2020. Retrieved 15 June 2020.
This article incorporates text from this source, which is in the public domain: Coronavirus (COVID-19) Update: FDA Warns of Newly Discovered Potential Drug Interaction That May Reduce Effectiveness of a COVID-19 Treatment Authorized for Emergency Use. U.S. Food and Drug Administration (FDA). 15 June 2020. Retrieved 15 June 2020.
- ^ "France bans use of hydroxychloroquine, drug touted by Trump, in coronavirus patients". CBS News. 27 May 2020.
- ^ Boseley S (16 June 202). "Recovery trial for Covid-19 treatments: what we know so far". The Guardian. Retrieved 21 June 2020.
- ^ WHO welcomes preliminary results about dexamethasone use in treating critically ill COVID-19 patients. World Health Organization (WHO). 16 June 2020. Retrieved 21 June 2020.
- ^ Q&A: Dexamethasone and COVID-19. World Health Organization (WHO). Retrieved 12 July 2020.
- ^ "Corticosteroids". COVID-19 Treatment Guidelines. National Institutes of Health. Retrieved 12 July 2020.
- ^ hdl:10665/334125. WHO/2019-nCoV/Corticosteroids/2020.1.
- ^ "WHO updates clinical care guidance with corticosteroid recommendations". World Health Organization (WHO). Retrieved 25 January 2022.
- S2CID 221467783.
- S2CID 221468015.
- ^ a b EMA endorses use of dexamethasone in COVID-19 patients on oxygen or mechanical ventilation. European Medicines Agency (EMA). 18 September 2020. Retrieved 21 September 2020. Text was copied from this source which is European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ Dexamethasone in hospitalised patients with COVID-19 (PDF) (Report). European Medicines Agency. 17 September 2020.
- ^ a b c
 This article incorporates text from this source, which is in the public domain: Coronavirus (COVID-19) Update: FDA Authorizes Monoclonal Antibody for Treatment of COVID-19. U.S. Food and Drug Administration (FDA). 9 November 2020. Retrieved 9 November 2020.
This article incorporates text from this source, which is in the public domain: Coronavirus (COVID-19) Update: FDA Authorizes Monoclonal Antibody for Treatment of COVID-19. U.S. Food and Drug Administration (FDA). 9 November 2020. Retrieved 9 November 2020.
- ^
 This article incorporates text from this source, which is in the public domain: FDA Authorizes Monoclonal Antibodies for Treatment of COVID-19. U.S. Food and Drug Administration (FDA). 10 February 2021. Retrieved 9 February 2021.
This article incorporates text from this source, which is in the public domain: FDA Authorizes Monoclonal Antibodies for Treatment of COVID-19. U.S. Food and Drug Administration (FDA). 10 February 2021. Retrieved 9 February 2021.
- ^
 This article incorporates text from this source, which is in the public domain: Coronavirus (COVID-19) Update: FDA Revokes Emergency Use Authorization for Monoclonal Antibody Bamlanivimab. U.S. Food and Drug Administration (FDA). 16 April 2021. Retrieved 16 April 2021.
This article incorporates text from this source, which is in the public domain: Coronavirus (COVID-19) Update: FDA Revokes Emergency Use Authorization for Monoclonal Antibody Bamlanivimab. U.S. Food and Drug Administration (FDA). 16 April 2021. Retrieved 16 April 2021.
- PMID 32282863.
- PMID 33203513.
- ^ Liu R, Miller J (3 March 2020). "China approves use of Roche drug in battle against coronavirus complications". Reuters. Archived from the original on 12 March 2020. Retrieved 14 March 2020.
- PMID 32350134.
- ^ Ovadia D, Agenzia Z. "COVID-19 – Italy launches an independent trial on tocilizumab". Univadis from Medscape. Aptus Health. Retrieved 22 April 2020.
- ^ "Tocilizumab in COVID-19 Pneumonia (TOCIVID-19) (TOCIVID-19)". clinicaltrials.gov. Retrieved 22 April 2020.
- ^ Various sources:
- "How doctors can potentially significantly reduce the number of deaths from Covid-19". Vox. 12 March 2020. Archived from the original on 19 March 2020. Retrieved 14 March 2020.
- Ruan Q, Yang K, Wang W, Jiang L, Song J (May 2020). "Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China". Intensive Care Medicine. 46 (5): 846–848. PMID 32125452.
- Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ (March 2020). "COVID-19: consider cytokine storm syndromes and immunosuppression". Lancet. 395 (10229): 1033–1034. PMID 32192578.
- ^ Slater H (26 March 2020). "FDA Approves Phase III Clinical Trial of Tocilizumab for COVID-19 Pneumonia". cancernetwork.com. Cancer Network. Retrieved 22 April 2020.
- S2CID 155698207.
- PMID 30463995.
- ^ PMID 32167489.
- ^ PMID 37162745.
- ^ PMID 32566896.
- PMID 33215063.
- PMID 34104626.
- S2CID 219552665.
- PMID 32151325.
- S2CID 223558059.
- PMID 32816541.
- PMID 32873684.
- PMID 32981770.
Further reading
- "Progress report on the coronavirus pandemic". Wikidata Q98568681.
- COVID-19 infection prevention and control measures for primary care, including general practitioner practices, dental clinics and pharmacy settings: first update. European Centre for Disease Prevention and Control (ECDC) (Report). October 2020.
- Erola Pairo-Castineira, Sara Clohisey, Lucija Klarić, Andrew Bretherick, Konrad Rawlik, Dorota Pasko, et al. (11 December 2020). "Genetic mechanisms of critical illness in Covid-19". Wikidata Q104287299..
{{cite journal}}: CS1 maint: numeric names: authors list (link) CS1 maint: overridden setting (link) Scholia Q104287299
External links
Health agencies
- Coronavirus (COVID‑19) by the UK National Health Service (NHS)
- Coronavirus 2019 (COVID-19) by the US Centers for Disease Control and Prevention (CDC)
- Coronavirus disease (COVID‑19) Facts by the World Health Organization (WHO)
Directories
- Coronavirus Resource Center at the Center for Inquiry
- COVID-19 at Curlie
- COVID‑19 Information on FireMountain.net Archived 13 January 2022 at the Wayback Machine
- COVID‑19 Resource Directory on OpenMD
Medical journals
- BMJ's Coronavirus (covid‑19) Hub by the BMJ
- Coronavirus (Covid‑19) by The New England Journal of Medicine
- Coronavirus (COVID‑19) Research Highlights by Springer Nature
- Coronavirus Disease 2019 (COVID‑19) by JAMA
- COVID‑19 Resource Centre by The Lancet
- Covid‑19: Novel Coronavirus Archived 24 September 2020 at the Wayback Machine by Wiley Publishing
- Novel Coronavirus Information Center by Elsevier
Treatment guidelines
- "Bouncing Back From COVID-19: Your Guide to Restoring Movement" (PDF). Johns Hopkins Medicine.
- "Coronavirus Disease 2019 (COVID-19) Treatment Guidelines" (PDF). National Institutes of Health.
- "Guidelines on the Treatment and Management of Patients with COVID-19". Infectious Diseases Society of America.
- "JHMI Clinical Recommendations for Available Pharmacologic Therapies for COVID-19" (PDF). Johns Hopkins Medicine.
- NHS England and NHS Improvement. National Guidance for post-COVID syndrome assessment clinics (Report).
- hdl:10665/351006. WHO/2019-nCoV/therapeutics/2022.1.
 Media from Commons
Media from Commons News from Wikinews
News from Wikinews Quotations from Wikiquote
Quotations from Wikiquote Resources from Wikiversity
Resources from Wikiversity Data from Wikidata
Data from Wikidata
| |
| General topics | |
| People | |
| In popular culture | |
| Related articles | |
| Upper RT (including URTIs, common cold) |
| ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||
| Pleural cavity/ mediastinum |
| ||||||||||||||||||||||
| Other/general | |||||||||||||||||||||||
| Oncovirus | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Immune disorders | |||||||||
| Central nervous system |
| ||||||||
| Cardiovascular | |||||||||
| Respiratory system/ acute viral nasopharyngitis/ viral pneumonia |
| ||||||||
| Human digestive system |
| ||||||||
| Urogenital | |||||||||

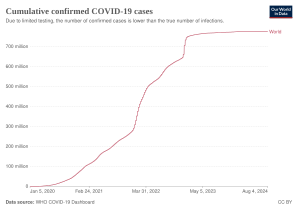
![Total confirmed cases of COVID‑19 per million people[348]](http://upload.wikimedia.org/wikipedia/commons/thumb/7/75/World_map_of_total_confirmed_COVID-19_cases_per_million_people.svg/298px-World_map_of_total_confirmed_COVID-19_cases_per_million_people.svg.png)
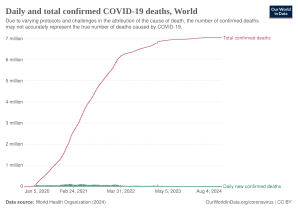
![Total confirmed deaths due to COVID‑19 per million people[349]](http://upload.wikimedia.org/wikipedia/commons/thumb/3/3a/World_map_of_total_confirmed_COVID-19_deaths_per_million_people_by_country.svg/298px-World_map_of_total_confirmed_COVID-19_deaths_per_million_people_by_country.svg.png)