Familial hypercholesterolemia
| Familial hypercholesterolemia | |
|---|---|
| Other names | Familial hypercholesterolaemia |
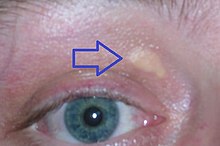 | |
| Xanthelasma palpebrarum, yellowish patches consisting of cholesterol deposits above the eyelids. These are more common in people with FH. | |
| Specialty | Endocrinology |
Familial hypercholesterolemia (FH) is a
FH is classified as a type 2 familial dyslipidemia.[1] There are five types of familial dyslipidemia (not including subtypes), and each are classified from both the altered lipid profile and by the genetic abnormality. For example, high LDL (often due to LDL receptor defect) is type 2. Others include defects in chylomicron metabolism, triglyceride metabolism, and metabolism of other cholesterol-containing particles, such as VLDL and IDL.
About 1 in 100 to 200 people have mutations in the LDLR gene that encodes the
Heterozygous FH is normally treated with statins,
Signs and symptoms
Physical signs
High cholesterol levels normally do not cause any symptoms. Yellow deposits of cholesterol-rich fat may be seen in various places on the body such as around the eyelids (known as xanthelasma palpebrarum), the outer margin of the iris (known as arcus senilis corneae), and in the tendons of the hands, elbows, knees and feet, particularly the Achilles tendon (known as a tendon xanthoma).[4][5]
Cardiovascular disease
Accelerated deposition of cholesterol in the walls of
Diagnosis
| Criteria for diagnosis of probable heterozygous FH
(98% specificity)[8] | ||||||
|---|---|---|---|---|---|---|
| 1st degree relative | general population | |||||
| age | cholesterol | mg/dL | mmol/L | mg/dL | mmol/L | |
| < 18 | total | > 220 | > 5.7 | > 270 | > 7.0 | |
| LDL-C | > 155 | > 4.0 | > 200 | > 5.2 | ||
| 20–29 | total | > 240 | > 6.2 | > 290 | > 7.5 | |
| LDL-C | > 170 | > 4.4 | > 220 | > 5.7 | ||
| 30–39 | total | > 270 | > 7.0 | > 340 | > 8.8 | |
| LDL-C | > 190 | > 5.0 | > 240 | > 6.2 | ||
| ≥ 40 | total | > 290 | > 7.5 | > 360 | > 9.3 | |
| LDL-C | > 205 | > 5.3 | > 260 | > 6.7 | ||
| First-degree relatives are parents, offspring, brothers, and sisters | ||||||
Approximately 85% of individuals with this disorder have not been diagnosed and consequently are not receiving lipid-lowering treatments.[9] Physical examination findings can help a physician make the diagnosis of FH. Tendon xanthomas are seen in 20-40% of individuals with FH and are pathognomonic for the condition.[9] A xanthelasma or corneal arcus may also be seen. These common signs are supportive of the diagnosis, but are non-specific findings.[9]
Lipid measurements
Mutation analysis
On the basis of the isolated high LDL and clinical criteria (which differ by country),
Differential diagnosis
FH needs to be distinguished from
This condition does not have increased blood cholesterol but the accumulation of cholesterol derivative in the tendon can mimic FH.Genetics
The most common genetic defects in FH are LDLR loss of function mutations (
LDL receptor


The
There are five major classes of FH due to LDLR mutations:[12]
- Class I: LDLR is not synthesized at all.
- Class II: LDLR is not properly transported from the endoplasmic reticulum to the Golgi apparatus for expression on the cell surface.
- Class III: LDLR does not properly bind LDL on the cell surface because of a defect in either apolipoprotein B100 (R3500Q) or in LDL-R.
- Class IV: LDLR bound to LDL does not properly cluster in clathrin-coated pits for receptor-mediated endocytosis (pathway step 2).
- Class V: LDLR is not recycled back to the cell surface (pathway step 5).
Apolipoprotein B
PCSK9
Mutations in the
LDLRAP1
Abnormalities in the ARH gene, also known as
Pathophysiology
LDL cholesterol normally circulates in the body for 2.5 days, and subsequently the apolipoprotein B portion of LDL cholesterol binds to the LDL receptor on the liver cells, triggering its uptake and digestion.[9] This process results in the removal of LDL from the circulatory system. Synthesis of cholesterol by the liver is suppressed in the HMG-CoA reductase pathway.[17] In FH, LDL receptor function is reduced or absent,[9] and LDL circulates for an average duration of 4.5 days, resulting in significantly increased level of LDL cholesterol in the blood with normal levels of other lipoproteins.[6] In mutations of ApoB, reduced binding of LDL particles to the receptor causes the increased level of LDL cholesterol. It is not known how the mutation causes LDL receptor dysfunction in mutations of PCSK9 and ARH.[4]
Although atherosclerosis occurs to a certain degree in all people, people with FH may develop accelerated atherosclerosis due to the excess level of LDL. The degree of atherosclerosis approximately depends on the number of LDL receptors still expressed and the functionality of these receptors. In many heterozygous forms of FH, the receptor function is only mildly impaired, and LDL levels will remain relatively low. In the more serious homozygous forms, the receptor is not expressed at all.[4]
Some studies of FH
Screening
Cholesterol screening and genetic testing among family members of people with known FH is
A 2007 meta-analysis found that "the proposed strategy of screening children and parents for familial hypercholesterolaemia could have considerable impact in preventing the medical consequences of this disorder in two generations simultaneously."[28] "The use of total cholesterol alone may best discriminate between people with and without FH between the ages of 1 to 9 years."[29][28]
Screening of toddlers has been suggested, and results of a trial on 10,000 one-year-olds were published in 2016. Work was needed to find whether screening was cost-effective, and acceptable to families.[30][31] Genetic counseling can help assist in genetic testing following a positive cholesterol screen for FH.[32]
Treatment
Heterozygous FH
Heterozygous familial hypercholesterolemia (HeFH) is usually treated with
More controversial is the addition of
There are no interventional studies that directly show mortality benefit of cholesterol lowering in FH. Rather, evidence of benefit is derived from a number of trials conducted in people who have polygenic hypercholesterolemia (in which heredity plays a smaller role). Still, a 1999 observational study of a large British registry showed that mortality in people with FH had started to improve in the early 1990s when statins were introduced.[36]
A cohort study suggested that treatment of FH with statins leads to a 48% reduction in death from coronary heart disease to a point where people are no more likely to die of coronary heart disease than the general population. However, if the person already had coronary heart disease the reduction was 25%. The results emphasize the importance of early identification of FH and treatment with statins.[37]
Alirocumab and evolocumab, both monoclonal antibodies against PCSK9, are specifically indicated as adjunct to diet and maximally tolerated statin therapy for the treatment of adults with heterozygous familial hypercholesterolemia, who require additional lowering of LDL cholesterol.[38]
More recently Inclisiran has been approved for the treatment of HeFH
Although monoclonal antibodies against PCSK9 is highly effective for patients with FH, the parenteral administration makes it less acceptable by the patient. There are many oral PCSK9 studied in the clinical trials (phase 2 and phase 3) and will be soon adopted as the treatment of hypercholesterolemia.
Homozygous FH
Homozygous familial hypercholesterolemia (HoFH) is harder to treat. The LDL (Low Density Lipoprotein) receptors are minimally functional, if at all. Only high doses of statins, often in combination with other medications, are modestly effective in improving lipid levels.
Lomitapide, an inhibitor of the microsomal triglyceride transfer protein,[45] was approved by the US FDA in December 2012 as an orphan drug for the treatment of homozygous familial hypercholesterolemia.[46] In January 2013, The US FDA also approved mipomersen, which inhibits the action of the gene apolipoprotein B, for the treatment of homozygous familial hypercholesterolemia.[47][48][49] Gene therapy is a possible future alternative.[50]
Evinacumab, a monoclonal antibody inhibiting angiopoietin-like protein 3, was approved in 2021 for adjunct therapy.[51]
Children
Given that FH is present from birth and atherosclerotic changes may begin early in life,
An expert panel in 2006 advised on early combination therapy with LDL apheresis, statins, and cholesterol absorption inhibitors in children with homozygous FH at the highest risk.[56]
Epidemiology
The global prevalence of FH is approximately 10 million people.[9] In most populations studied, heterozygous FH occurs in about 1:250 people, but not all develop symptoms.[3] Homozygous FH occurs in about 1:1,000,000.[4][6]
LDLR mutations are more common in certain populations, presumably because of a genetic phenomenon known as the
History
The Norwegian physician Dr Carl Müller first associated the physical signs, high cholesterol levels and autosomal dominant inheritance in 1938.
See also
- Primary hyperlipoproteinemia
- Familial hypertriglyceridemia
- Lipoprotein lipase deficiency
- Familial apoprotein CII deficiency
- Akira Endo, discoverer of the first statin
References
- PMID 25598733.
- PMID 21600525.
- ^ PMID 28864697.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ PMID 12813012.
- S2CID 38952905.
- ^ S2CID 208792416.
- S2CID 25292760.
- PMID 8328379.
- ^ PMID 24481802.
- PMID 16825289.
- PMID 11939886.
- ^ S2CID 5756814.
- PMID 3771801.
- S2CID 19462210.
- S2CID 22395543.
- PMID 4351242.
- PMID 4362634.
- PMID 1933004.
- PMID 11325764.
- PMID 15879303.
- S2CID 27054208.
- PMID 2139920.
- PMID 9603531.
- PMID 26115072.
- PMID 12039822.
- S2CID 25342898.
- PMID 12669918.
- ^ PMID 17855284.
- PMID 22510399.
- ^ Caroline Parkinson (27 October 2016). "Toddlers 'should get heart risk test'". BBC News. Retrieved 27 October 2016.
- PMID 27783906.

- ^ "Genetic Counseling for Familial Hypercholesterolemia | CDC". www.cdc.gov. 2020-04-01. Retrieved 2021-02-12.
- PMID 21191428.
- National Institute for Health and Clinical Excellence. Clinical guideline 71: Familial hypercholesterolaemia. London, 2008.
- S2CID 8085257. Archived from the original(PDF) on 2020-06-29.
- PMID 9920511.
- PMID 18840879.
- PMID 27195910.
- S2CID 8075552.
- PMID 6390206.
- PMID 8554367.
- PMID 10770402.
- S2CID 27446759.
- PMID 172531.
- PMID 17215532.
- ^ "FDA approves new orphan drug for rare cholesterol disorder" (Press release). U.S. Food and Drug Administration. 26 December 2012. Archived from the original on 31 December 2012.
- PMID 34357325.
- ^ Pollack A (29 January 2013). "F.D.A. Approves Genetic Drug to Treat Rare Disease". The New York Times.
- ^ "FDA approves new orphan drug Kynamro to treat inherited cholesterol disorder" (Press release). U.S. Food and Drug Administration. 29 January 2013. Archived from the original on 2 February 2013.
- S2CID 3194865.
- FDA. 13 May 2022.
- PMID 2914343.
- ^ PMID 15121812.
- S2CID 38754088.
- PMID 15265847.
- PMID 17130340.
- .
- PMID 4355366.
- PMID 174194.
- ^ Nobelprize.org. "Medicine 1985". Retrieved 2008-02-28.
External links
