Tropical spastic paraparesis
| Tropical spastic paraparesis | |
|---|---|
| Other names | HTLV-I-associated myelopathy (HAM) or HTLV-I-associated myelopathy/tropical spastic paraparesis (HAM/TSP)[1] |
 | |
| HTLV-1 which causes TSP | |
| Specialty | Neurology |
| Symptoms | Bowel dysfunction[2] |
| Causes | HTLV-1 retrovirus causes 80% of cases[3] |
| Diagnostic method | Lumbar puncture, MRI[2] |
| Treatment | Interferon alpha, corticosteroids[3] |
Tropical spastic paraparesis (TSP), is a medical condition that causes weakness,
Signs and symptoms
Some of the signs of Tropical spastic paraparesis are:[2]
- Leg instability
- Urinary dysfunction.
- Bowel dysfunction
- Back pain
- Erectile problems
- Psoriasis
Individuals with TSP may also exhibit
HTLV-1 can be transmitted via breastfeeding (mother to child), sexual contact, via blood contact (transfusion or needle sharing).[7]
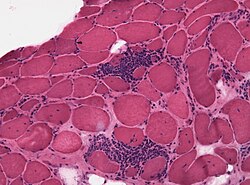
Pathogenesis
In tropical spastic paraparesis, HTLV-1 shows elevated cellular acquired immune response as well as high production of
Diagnosis
Among the methods of diagnosing tropical spastic paraparesis are
Often, the diagnosis process is based on symptoms and one's risk of exposure to the virus. A spinal tap or lumbar puncture may be used to obtain blood and CSF samples which can then be tested for parts of the virus or antibodies produced to combat the virus. MRI may be performed on the brain and spinal cord to check for abnormalities such as spinal cord degeneration and other potential causes of symptoms.[9]
Treatment

Treatment of TSP involves
Prognosis
The prognosis for tropical spastic paraparesis indicates some improvement in a percentage of cases due to immunosuppressive treatment. A higher percentage will eventually lose the ability to walk within a ten-year interval.[12]
History
For several decades, the term tropical spastic paraparesis was used to describe a chronic and progressive clinical syndrome that affected adults living in equatorial areas of the world. This condition was initially thought to be associated with infectious agents (such as
See also
- Treponema pallidum
- Myelopathy
- Lymphatic system
- Neuropathy
References
- PMID 18657726.
- ^ a b c d "Tropical Spastic Paraparesis. About TSP medical condition | Patient". Patient. Archived from the original on 29 November 2017. Retrieved 24 July 2016.
- ^ a b "Tropical Spastic Paraparesis Information Page | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. Archived from the original on 23 October 2018. Retrieved 3 January 2018.
- ^ "Tropical Spastic Paraparesis Information Page: National Institute of Neurological Disorders and Stroke (NINDS)". www.ninds.nih.gov. Archived from the original on 2016-12-15. Retrieved 2015-08-13.
- from the original on 2019-04-03. Retrieved 2017-09-17.
- ISBN 9781444356359. Archivedfrom the original on 2023-01-11. Retrieved 2020-11-07.
- ^ "HTLV-1 associated myelopathy/tropical spastic paraparesis | Disease | Overview | Office of Rare Diseases Research (ORDR-NCATS)". rarediseases.info.nih.gov. Archived from the original on 2015-09-05. Retrieved 2015-08-13.
- PMID 23162542.
- ^ "HTLV-1–Associated Myelopathy/Tropical Spastic Paraparesis (HAM/TSP)". Merck Manual Consumer Version. Archived from the original on 28 February 2023. Retrieved 28 February 2023.
- PMID 17691249.
- ^ Human T-Cell Lymphotropic Viruses~treatment at eMedicine
- ISBN 978-1437709490. Archivedfrom the original on 2023-01-11. Retrieved 2020-11-07.
- ^ Tropical Myeloneuropathies at eMedicine
Further reading
- Machigashira, N.; Yoshida, Y.; Wang, S.-y.; Osame, M. (2001). "HTLV-1-associated myelopathy/tropical spastic paraparesis with pseudohypoparathyroidism". Neurology. 56 (1): 104–6. PMID 11148245.
- Nagamine, Yuito; Hayashi, Takeshi; Kato, Yuji; Horiuchi, Yohsuke; Tanahashi, Norio (2015). "Human T Lymphotropic Virus Type-1-associated Myelopathy Manifesting Shortly after Living-donor Renal Transplantation". Internal Medicine. 54 (1): 75–8. PMID 25742898.