Nasopharyngeal carcinoma
| Nasopharyngeal carcinoma | |
|---|---|
| Other names | Nasopharyngeal cancer, nasopharynx cancer, NPC |
 | |
| Micrograph showing a nasopharyngeal carcinoma positive for Epstein-Barr virus-encoded small RNAs (EBER). | |
| Specialty | Oncology |
Nasopharyngeal carcinoma (NPC), or nasopharynx cancer, is the most common
Signs and symptoms
NPC may present as a lump or a mass on both sides towards the back of the neck. These lumps usually are not tender or painful but appear as a result of the metastatic spread of the cancer to the lymph nodes, thus causing the lymph nodes to swell. Lymph nodes are defined as glands that function as part of the immune system and can be found throughout the body.
Causes
NPC is caused by a combination of factors: viral, environmental influences, and heredity.
The association between Epstein-Barr virus and nasopharyngeal carcinoma is unequivocal in World Health Organization (WHO) types II and III tumors but less well-established for WHO type I (WHO-I) NPC, where preliminary evaluation has suggested that
It is also being investigated as to whether or not chronic sinusitis could be a potential cause of cancer of the nasopharynx. It is hypothesised that this may happen in a way similar to how chronic inflammatory conditions in other parts of the body, such as esophagitis sometimes leading to Barrett's esophagus because of conditions such as gastroesophageal reflux disease.[12]
Diagnosis
Classification
The World Health Organization (WHO) has identified three subtypes of nasopharyngeal carcinoma:[citation needed]
- type 1: squamous cell carcinoma, typically found in older adults
- type 2: non-keratinizing carcinoma
- type 3: undifferentiated carcinoma
Type 3 is most commonly found among younger children and adolescents, with a few type 2 cases. Both type 2 and 3 have been found to be associated with elevated levels of Epstein-Barr virus titers, but not type 1. Additionally, type 2 and type 3 may be followed with an influx of inflammatory cells, including lymphocytes, plasma cells, and eosinophils – a condition referred to as lymphoepithelioma.[13]
Nasopharyngeal carcinoma, also known as nasopharyngeal cancer, is classified as a malignant
-
Undifferentiated nasopharyngeal carcinoma—low power
-
Undifferentiated nasopharyngeal carcinoma—med. power
-
Undifferentiated nasopharyngeal carcinoma—high power
-
Undifferentiated nasopharyngeal carcinoma—high power
Staging
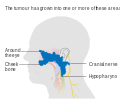
Staging of nasopharyngeal carcinoma is based on clinical and radiologic examination. Most patients present with Stage III or IV disease.
Stage I is a small tumor confined to nasopharynx.
Stage II is a tumor extending in the local area, or that with any evidence of limited neck (nodal) disease.
Stage III is a large tumor with or without neck disease, or a tumor with bilateral neck disease.
Stage IV is a large tumor involving intracranial or infratemporal regions, an extensive neck disease, and/or any distant metastasis. [16]
-
Stage T1 nasopharyngeal cancer
-
Stage T2 nasopharyngeal cancer
-
Stage T3 nasopharyngeal cancer
-
Stage T4 nasopharyngeal cancer
Risk factors
Nasopharyngeal carcinoma, classified as a squamous cell cancer, has not been linked to excessive use of tobacco. However, there are certain risk factors that can predispose an individual to NPC if exposed to them. These risk factors include: having Chinese, or Asian, ancestry, exposure to Epstein- Barr virus (EBV), unknown factors that result in rare familial clusters, and heavy alcohol consumption.[17]
EBV
Epstein- Barr virus infects and persists in more than 90% of world population. Transmission of this virus occurs through saliva and is more commonly seen in developing countries where there are living areas are more packed together and less hygienic. Replication of this virus can occur in the oropharyngeal epithelial tissue and nasopharyngeal tissue. EBV primarily targets B lymphocytes. Patients diagnosed with NPC were found to show elevated levels of the antibodies against the EBV antigen than in individuals not diagnosed with NPC.[18]
Smoking
Individuals that are exposed to cigarette smoking have an increased risk of developing NPC by 2- to 6-fold. Approximately two-thirds of patients with type 1 NPC was attributed to smoking in the United States. However the declining rates of smoking in the US can be associated with less prevalence of type 1 NPC. In southern China and North Africa, it has been suggested that high smoking rates come from wood fires in the country rather than cigarette smoking.[18]
Treatment
NPC can be treated by surgery, by chemotherapy, radiotherapy,[19] or by immunotherapy.[20] There are different forms of radiation therapy, including 3D conformal radiation therapy, intensity-modulated radiation therapy, particle beam therapy and brachytherapy, which are commonly used in the treatments of cancers of the head and neck. The expression of EBV latent proteins within undifferentiated nasopharyngeal carcinoma can be potentially exploited for immune-based therapies.[21] Generally, there are three different types or treatment methods that can be used for patients with nasopharyngeal carcinoma. These three treatments are radiation therapy, chemotherapy, and surgery. Although there are currently three treatment methods, there are clinical trials taking place that may develop more effective treatments for NPC. A clinical trial is research study that works to develop new treatment techniques or to gain more information about or improve current methods. If an effective treatment comes out of the clinical trial, then this method may become a new standard treatment method. During the course of, or following, treatment, tests may be done in order to determine if the treatment is working, or if treatment needs to be dropped or changed. Tests that are done after treatment to determine the condition of patient after completing treatment are called follow-up tests and tell the doctor if the patient's condition has changed or if the cancer has come back.[22]
Radiation therapy
Radiation therapy uses high energy x-rays or other types of radiation aimed to prevent cancer cells from growing or kill them altogether. This kind of therapy can be administered to the patient externally or internally. With external radiation, a machine is used to send targeted radiation to the cancer site. A mesh mask is used on the patient in order to keep their head and neck still while the machine rotates to send out beams of radiation. In undergoing this kind of treatment, healthy cells may also be damaged during the process. Therefore, there are 2 other forms of radiation therapy that decreases the likelihood of damaging nearby healthy cells: intensity-modulated radiation therapy and stereotactic radiation therapy. Intensity-modulated radiation therapy (IMRT) uses 3D images of the size and shape of the tumor to then direct thin beams of radiation at different intensities from multiple angles. In stereotactic radiation therapy, radiation is aimed directly at the tumor. In this therapy, the total amount of radiation is divided into smaller doses that will be given over the course of several days. [citation needed]
Using radiation therapy as a cancer treatment method depends on the type and stage of cancer; however, internal and external radiation therapies can be used to treat NPC. If external radiation therapies are being aimed at the thyroid, then this could affect the way the thyroid works. For that reason, blood tests are done before and after radiation to check thyroid hormone levels.[22]
Chemotherapy
Chemotherapy works as cancer treatment by using drugs that stop the growth of cancer cells, by either killing the cells or preventing them from dividing. This kind of therapy can be administered systemically or regionally. Systemic chemotherapy is when the chemotherapy is taken orally or is injected into a vein or muscle. In this method, the drug circulates through the blood system and can reach cancer cells throughout the body. Regional chemotherapy is when chemotherapy is administered directly into the cerebrospinal fluid, an organ, or a body cavity, for example, the abdomen. In this way, the drugs will mainly affect cancer cells in that area. However, the type of chemotherapy that is administered to the patient depends on the type and stage of the cancer. Additionally, chemotherapy can be used as an adjuvant therapy after radiation to lower the risk of recurrence in the patient. If given after radiation, chemotherapy can be used to kill any cancer cells that may have remained.[22]
Immunotherapy
The Food and Drug Administration approved toripalimab-tpzi (LOQTORZ, Coherus BioSciences, Inc.) with cisplatin and gemcitabine for the first-line treatment of adults with metastatic or recurrent, locally advanced nasopharyngeal carcinoma (NPC). FDA also approved toripalimab-tpzi as a single agent for adults with recurrent unresectable or metastatic NPC with disease progression on or after a platinum-containing chemotherapy.[23]
Surgery
Surgery can be used as a method to determine whether there is cancer present or to remove cancer from the body. If the tumor does not respond to radiation therapy, then the patient may undergo an operation to have it removed. Cancers that may have spread to the lymph nodes may require the doctor to remove lymph nodes or other tissue in the neck.[22]
Epidemiology
As of 2010, NPC resulted in 65,000 deaths globally up from 45,000 in 1990.[24]
NPC is uncommon in the
See also
References
- S2CID 29670301.
- ^ a b "Signs and Symptoms of Nasopharyngeal Cancer". www.cancer.org. Retrieved 2020-04-27.
- ^ "Nasopharyngeal Cancer Treatment (Adult) (PDQ®)–Patient Version - National Cancer Institute". www.cancer.gov. 2020-04-13. Retrieved 2020-04-27.
- PMID 11593591.
- ^ a b "Initiative for Vaccine Research (IVR): Viral cancers". World Health Organization. Archived from the original on 1 April 2019. Retrieved 2 October 2012.
- ^ PMID 22245473.
- PMID 3940655.
- ^ PMID 17035381.
- PMID 28098136.
- PMID 20824783.
- ^ S2CID 10765689.
- S2CID 30791737.
- PMID 16800883.
- ISBN 978-92-832-2438-9.
- ^ ISBN 978-0-7216-7253-3.[page needed]
- ^ AJCC Cancer Staging Manual (7th ed.). New York, NY: Springer. 2010. pp. 41–56.
- PMID 26389193, retrieved 2020-04-28
- ^ PMID 17035381.
- PMID 16800883.
- ^ Research, Center for Drug Evaluation and (2023-10-30). "FDA approves toripalimab-tpzi for nasopharyngeal carcinoma". FDA.
- S2CID 7615720.
- ^ a b c d "Nasopharyngeal Cancer Treatment (Adult) (PDQ®)–Patient Version - National Cancer Institute". www.cancer.gov. 2020-04-13. Retrieved 2020-04-27.
- ^ Research, Center for Drug Evaluation and (2023-10-30). "FDA approves toripalimab-tpzi for nasopharyngeal carcinoma". FDA.
- S2CID 1541253.
- PMID 18570662.
- PMID 20426903.
External links
- Cancer Management Handbook: Head and Neck Tumors Archived 2013-10-04 at the Wayback Machine
- Clinically reviewed nasopharyngeal cancer information for patients from Cancer Research UK