Levonorgestrel
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Plan B, Julie, Mirena, Plan B One-Step, Liletta, others |
| Other names | LNG; LNG-EC; d-Norgestrel; d(–)-Norgestrel; D-Norgestrel; WY-5104; SH-90999; NSC-744007; 18-Methylnorethisterone; 17α-Ethynyl-18-methyl-19-nortestosterone; 17α-Ethynyl-18-methylestr-4-en-17β-ol-3-one; 13β-Ethyl-17α-hydroxy-18,19-dinorpregn-4-en-20-yn-3-one |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a610021 |
| Pregnancy category | |
Progestin | |
| ATC code | |
| Legal status | |
| Legal status | |
| Metabolites | • 5α-Dihydro-LNG[4] |
| Elimination half-life | 24–32 hours[4] |
| Excretion | Urine: 20–67% Feces: 21–34%[6] |
| Identifiers | |
| |
JSmol) | |
| Melting point | 235 to 237 °C (455 to 459 °F) |
| |
| |
| (verify) | |
Levonorgestrel is a
Common
Levonorgestrel was patented in 1960 and introduced for medical use together with
Medical uses
Birth control
At low doses, levonorgestrel is used in
At very low daily dose of 30 µg, levonorgestrel is used in some
Levonorgestrel is the active ingredient in a number of
One of the more common forms of contraception that contains only levonorgestrel is an IUD. One IUD, the Mirena, is a small hollow cylinder containing levonorgestrel and polydimethylsiloxane and covered with a release rate controlling membrane.[21]
Emergency birth control
Levonorgestrel is used in
The primary mechanism of action of levonorgestrel as a progestogen-only emergency contraceptive pill is, according to
Other studies still find the evidence to be unclear.[30] While it is unlikely that emergency contraception affects implantation it is impossible to completely exclude the possibility of post-fertilization effect.[31]
In November 2013, the EMA also approved a change to the label for
An analysis of four WHO randomised clinical trials, published in January 2017, showed pregnancy rates of 1.25% (68/5428) in women with BMI under 25, 0.61% (7/1140) in women with BMI between 25 and 30, and 2.03% (6/295) in women with BMI over 30.[34] These values yield an eight-fold reduction in efficacy for women with BMI over 30 compared to women with BMI under 25. However, emergency contraceptives remain effective regardless of BMI.
Hormone therapy
Levonorgestrel is used in combination with an
Available forms
As a type of emergency contraception, levonorgestrel is used after unprotected intercourse to reduce the risk of pregnancy.[36] However, it can serve different hormonal purposes in its different methods of delivery. It is available for use in a variety of forms:
By mouth
Levonorgestrel can be taken by mouth as a form of emergency birth control. The typical dosage is either 1.5 mg taken once or 0.75 mg taken 12–24 hours apart.[37] The effectiveness in both methods is similar.[37] The most widely used form of oral emergency contraception is the progestin-only pill, which contains a 1.5 mg dosage of levonorgestrel.[36] Levonorgestrel-only emergency contraceptive pills are reported to have an 89% effectiveness rate if taken within the recommended 72 hours after sex.[38] The efficacy of the drug decreases by 50% for each 12-hour delay in taking the dose after the emergency contraceptive regimen has been started.[38]
Skin patch
Estradiol with levonorgestrel in the form of a skin patch is used under the brand name Climara Pro for hormone replacement therapy in postmenstrual women, treating symptoms such as hot flashes or osteoporosis.[39] The simultaneous delivery of a progestogen such as levonorgestrel is necessary for the protection of the endometrium.[40][41]
Intrauterine device
The levonorgestrel intrauterine system (LNG-IUS) is a type of long-term birth control that releases the progestin into the uterine cavity.[42][21] Levonorgestrel is released at a constant, gradual rate of 0.02 mg per day by the polydimethylsiloxane membrane of the device, which renders it effective for up to five years.[42] Because it is inserted directly into the uterus, levonorgestrel is present in the endometrium in much higher concentrations that would result from a LNG-containing oral pill; the LNG-IUS delivers 391 ng of levonorgestrel to the inner uterine region while a comparable oral contraceptive delivers only 1.35 ng.[42] This high level of levonorgestrel impedes the function of the endometrium, making it hostile for sperm transport, fertilization, and implantation of an ovum.[42]
Implant
Contraindications
Known or suspected pregnancy is a contraindication of levonorgestrel as an emergency contraceptive.[44]
Side effects
After an intake of 1.5 mg levonorgestrel in
Levonorgestrel as a contraceptive intrauterine device is associated with a higher risk of breast cancer than with non-use.[47]
Overdose
Interactions
If taken together with drugs that induce the CYP3A4 cytochrome P450 liver enzyme, levonorgestrel may be metabolized faster and may have lower effectiveness.[48] These include, but are not limited to barbiturates, bosentan, carbamazepine, felbamate, griseofulvin, oxcarbazepine, phenytoin, rifampin, St. John's wort and topiramate.[medical citation needed]
Pharmacology
Pharmacodynamics
Levonorgestrel is a
| Compound | PR | AR | ER | GR | MR | SHBG | CBG
|
|---|---|---|---|---|---|---|---|
| Levonorgestrel | 150–162 | 34a, 45 | 0 | 1–8 | 17–75 | 50 | 0 |
| 5α-Dihydrolevonorgestrel | 50 | 38a | 0 | ? | ? | ? | ? |
| 3α,5α-Tetrahydrolevonorgestrel | ? | ? | 0.4 | ? | ? | ? | ? |
| 3β,5α-Tetrahydrolevonorgestrel | ? | ? | 2.4 | ? | ? | ? | ? |
| Notes: Values are percentages (%). Reference CBG . Sources: See template.
| |||||||
Progestogenic activity
Levonorgestrel is a
Antigonadotropic effects
Due to its progestogenic activity, levonorgestrel has
In men, levonorgestrel causes marked suppression of circulating testosterone levels secondary to its antigonadotropic effects.
Androgenic activity
Levonorgestrel is a weak agonist of the
In combination with a potent estrogen like ethinylestradiol however, all contraceptives containing androgenic progestins are negligibly androgenic in practice and in fact can be used to treat androgen-dependent conditions like acne and hirsutism in women.[56] This is because ethinylestradiol causes a marked increase in SHBG levels and thereby decreases levels of free and hence bioactive testosterone, acting as a functional antiandrogen.[56] Nonetheless, contraceptives containing progestins that are less androgenic increase SHBG levels to a greater extent and may be more effective for such indications.[56] Levonorgestrel is currently the most androgenic progestin that is used in contraceptives, and contraceptives containing levonorgestrel may be less effective for androgen-dependent conditions relative to those containing other progestins that are less androgenic.[57][58][59]
Other activity
Levonorgestrel stimulates the
Pharmacokinetics
The
Chemistry
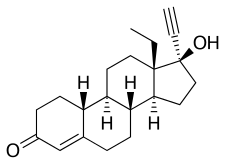
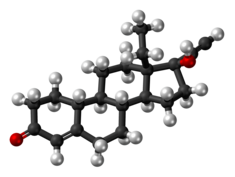
Levonorgestrel, also known as 17α-ethynyl-18-methyl-19-nortestosterone or as 17α-ethynyl-18-methylestr-4-en-17β-ol-3-one, is a
History
Levonorgestrel, taken alone in a single high dose, was first evaluated as a form of
Levonorgestrel has also been introduced for use as a
Society and culture
Generic names
Levonorgestrel is the
Brand names
Levonorgestrel is marketed alone or in combination with an
As an emergency contraceptive, levonorgestrel is often referred to colloquially as the "morning-after pill".[98][99]
Availability
Levonorgestrel is very widely marketed throughout the world and is available in almost every country.[19][64]
Accessibility
Levonorgestrel-containing emergency contraception is available
A policy update in 2015, required all pharmacies, clinics, and emergency departments run by
Research
Levonorgestrel has been studied in combination with
References
- ^ a b "Levonorgestrel Use During Pregnancy". Drugs.com. 23 March 2020. Archived from the original on 2 July 2020. Retrieved 29 June 2020.
- ^ "Jaydess 13.5 mg intrauterine delivery system - Summary of Product Characteristics (SmPC)". (emc). 1 July 2022. Archived from the original on 13 April 2021. Retrieved 1 July 2022.
- ^ a b c "Plan B One-Step- levonorgestrel tablet". DailyMed. 21 December 2022. Retrieved 26 December 2022.
- ^ S2CID 24616324.
- ^ PMID 8842581.
- ^ ISBN 978-1-4612-2730-4. Archivedfrom the original on 28 August 2021. Retrieved 15 April 2018.
- ^ a b c d e f g h i j k l "Progestins (Etonogestrel, Levonorgestrel, Norethindrone)". The American Society of Health-System Pharmacists. Archived from the original on 2015-09-07. Retrieved Aug 21, 2015.
- ISBN 9789350250822. Archivedfrom the original on 2015-09-26.
- ^ "Levonorgestrel 1.5 mg Tablet Emergency Contraceptive: New Drug Application 21998, Supplement 5" (PDF). U.S. Food and Drug Administration.
- ^ "Now Is the Time to Change Label on Emergency Contraceptives". Relias Media | Online Continuing Medical Education | Relias Media - Continuing Medical Education Publishing. Retrieved 2022-08-16.
- PMID 20933113.
- ISBN 9789241562089. Archivedfrom the original on 2015-09-26.
- ISBN 9783527607495. Archivedfrom the original on 2021-08-28. Retrieved 2020-08-05.
- ^ ISBN 978-3-527-33739-2. Archivedfrom the original on 2021-08-28. Retrieved 2018-04-18.
[Levonorgestrel (24): The product generated by Smith's norgestrel total synthesis was a racemate, so half of each consisted of the left- and the right-handed enantiomer. Chemists at Schering discovered that only the levorotatory enantiomer was effective [49] and developed a biotechnological process for the preparation of the pure levorotatory enantiomer. This was the active ingredient levonorgestrel born. With the single-acting enantiomer, the dose and thus the liver burden could be halved again. The resulting Neogynon® contained 0.25 mg levonorgestrel and 0.05 mg ethinylestradiol and was introduced in 1970.]
- hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ISBN 9781284053999. Archivedfrom the original on 2015-09-26.
- ^ "FDA approves Plan B One-Step emergency contraceptive for use without a prescription for all women of child-bearing potential" (Press release). June 20, 2013. Archived from the original on 14 January 2016. Retrieved 2 February 2016.
- ^ "Levonorgestrel - Drug Usage Statistics". ClinCalc. Retrieved 7 October 2022.
- ^ a b c d e f g h i j k l m n o p "Levonorgestrel". Archived from the original on 2017-08-03. Retrieved 2017-08-03.
- ^ PMID 26732558.
- ^ PMID 30195080.
- ^ "How often can you take the morning-after pill?". www.plannedparenthood.org. Archived from the original on 2022-06-24. Retrieved 2022-06-18.
- OCLC 781956734. p. 121:
Mechanism of action
Copper-releasing IUCs
When used as a regular or emergency method of contraception, copper-releasing IUCs act primarily to prevent fertilization. Emergency insertion of a copper IUC is significantly more effective than the use of ECPs, reducing the risk of pregnancy following unprotected intercourse by more than 99%.2,3 This very high level of effectiveness implies that emergency insertion of a copper IUC must prevent some pregnancies after fertilization.
Emergency contraceptive pills
To make an informed choice, women must know that ECPs—like the birth control pill, patch, ring, shot, and implant,76 and even like breastfeeding77—prevent pregnancy primarily by delaying or inhibiting ovulation and inhibiting fertilization, but may at times inhibit implantation of a fertilized egg in the endometrium. However, women should also be informed that the best available evidence indicates that ECPs prevent pregnancy by mechanisms that do not involve interference with post-fertilization events.
ECPs do not cause abortion78 or harm an established pregnancy. Pregnancy begins with implantation according to medical authorities such as the US FDA, the National Institutes of Health79 and the American College of Obstetricians and Gynecologists (ACOG).80
Ulipristal acetate (UPA). One study has demonstrated that UP can delay ovulation.81... Another study found that UPA altered the endometrium, but whether this change would inhibit implantation is unknown.82
p. 122:
Progestin-only emergency contraceptive pills. Early treatment with ECPs containing only the progestin levonorgestrel has been shown to impair the ovulatory process and luteal function.83–87
p. 123:
Combined emergency contraceptive pills. Several clinical studies have shown that combined ECPs containing ethinyl estradiol and levonorgestrel can inhibit or delay ovulation.107–110 - ISSN 1755-103X. Archived from the original(PDF) on 2012-05-26. Retrieved 2012-04-30. p.3:
How does EC work?
In 2002, a judicial review ruled that pregnancy begins at implantation, not fertilisation.8 The possible mechanisms of action should be explained to the patient as some methods may not be acceptable, depending on individual beliefs about the onset of pregnancy and abortion.
Copper-bearing intrauterine device (Cu-IUD). Copper is toxic to the ovum and sperm and thus the copper-bearing intrauterine device (Cu-IUD) is effective immediately after insertion and works primarily by inhibiting fertilisation.9–11 A systematic review on mechanisms of action of IUDs showed that both pre- and postfertilisation effects contribute to efficacy.11 If fertilisation has already occurred, it is accepted that there is an anti-implantation effect,12,13
Levonorgestrel (LNG). The precise mode of action of levonorgestrel (LNG) is incompletely understood but it is thought to work primarily by inhibition of ovulation.16,17
Ulipristal acetate (UPA). UPA's primary mechanism of action is thought to be inhibition or delay of ovulation.2 - ^ UNDP/UNFPA/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP) (March 25, 2010). "Fact sheet on the safety of levonorgestrel-alone emergency contraceptive pills (LNG ECPs)" (PDF). Geneva: World Health Organization. Archived (PDF) from the original on March 16, 2012.
Can LNG ECPs cause an abortion?
LNG ECPs do not interrupt an established pregnancy or harm a developing embryo.15 The evidence available to date shows that LNG ECP use does not prevent a fertilized egg from attaching to the uterine lining. The primary mechanism of action is to stop or disrupt ovulation; LNG ECP use may also prevent the sperm and egg from meeting.16 - ISBN 978-1-60831-610-6. p. 155:
Emergency postcoital contraception
Levonorgestrel
Mechanism and efficacy - ^ Belluck P (June 6, 2012). "No abortion role seen for morning-after pill". The New York Times. p. A1. Archived from the original on February 27, 2017.
Belluck P (June 6, 2012). "Drug's nickname may have aided politicization". The New York Times. p. A14. - International Federation of Gynecology and Obstetrics (FIGO) and International Consortium for Emergency Contraception (ICEC) (April 4, 2011). "Mechanism of action: How do levonorgestrel-only emergency contraceptive pills (LNG ECPs) prevent pregnancy?" (PDF). London: International Federation of Gynecology and Obstetrics. Archived(PDF) from the original on December 29, 2014.
Levonorgestrel-only emergency contraceptive pills:
• Interfere with the process of ovulation;
• May possibly prevent the sperm and the egg from meeting.
Implications of the research:
• Inhibition or delay of ovulation is LNG ECPs principal and possibly only mechanism of action.
• Review of the evidence suggests that LNG-ECs cannot prevent implantation of a fertilized egg. Language on implantation should not be included in LNG ECP product labeling.
• The fact that LNG-ECs have no demonstrated effect on implantation explains why they are not 100% effective in preventing pregnancy, and are less effective the later they are taken. Women should be given a clear message that LNG-ECs are more effective the sooner they are taken.
• LNG ECPs do not interrupt a pregnancy (by any definition of the beginning of pregnancy). However, LNG ECPs can prevent abortions by reducing unwanted pregnancies. - ^ HRA Pharma (November 2013). "NorLevo 1.5 mg tablet Summary of Product Characteristics (SPC)". Dublin: Irish Pharmaceutical Healthcare Association. Archived from the original on June 15, 2012. Retrieved March 5, 2014.from the original on March 27, 2014. Retrieved March 5, 2014.
European Medicines Agency (January 24, 2014). "Review of emergency contraceptives started". London: European Medicines Agency. Archived - S2CID 6431709.
- S2CID 41337748.
- PMID 21920190.
- ^ Trussell J, Raymond EG, Cleland K (February 2014). "Emergency contraception: a last chance to prevent unintended pregnancy" (PDF). Princeton: Office of Population Research at Princeton University, Association of Reproductive Health Professionals. Archived from the original (PDF) on September 23, 2010. Retrieved April 9, 2014.
- PMID 27527670.
- ^ a b c Kubíková D (2014). "[Menopausal symptoms and hormone replacement therapy]" (PDF). Praktické Lékárenství. 10 (2): 68–73.
- ^ a b "Emergency Contraception - ACOG". www.acog.org. Archived from the original on 2019-10-09. Retrieved 2019-06-01.
- ^ S2CID 24229915.
- ^ PMID 24708837.
- ^ "Estradiol And Levonorgestrel (Transdermal Route) Description and Brand Names - Mayo Clinic". www.mayoclinic.org. Archived from the original on 2019-05-31. Retrieved 2019-06-01.
- ^ "Climara Pro® (Estradiol/Levonorgestrel Transdermal System)" (PDF). Food and Drug Administration. Archived (PDF) from the original on 2021-02-28. Retrieved 2019-06-01.
- S2CID 51886877.
- ^ S2CID 43177026.
- S2CID 207201811.
- ^ a b c "Plan B One-Step (levonorgestrel) tablet, 1.5 mg, for oral use" (PDF). Barr Pharmaceuticals, Inc. U.S. Food and Drug Administration. July 2009. Archived from the original (PDF) on 2019-04-17.
- HRA Pharma (November 2013). "NorLevo 1.5 mg tablet Summary of Product Characteristics (SPC)". Dublin: Irish Pharmaceutical Healthcare Association. Archived from the originalon June 15, 2012. Retrieved April 9, 2014.
- PMID 24708811.
- S2CID 210946832.
- ^ Medicines and Healthcare products Regulatory Agency (15 September 2016). "Levonorgestrel-containing emergency hormonal contraception: advice on interactions with hepatic enzyme inducers and contraceptive efficacy". GOV.UK. Archived from the original on 21 January 2017. Retrieved 6 June 2017.
- ^ PMID 14670641.
- ISBN 978-3-642-95583-9.
- PMID 2215269.
- ^ (PDF) from the original on 2020-12-05. Retrieved 2019-07-11.
- PMID 22078182.
- ^ PMID 12826683.
Based on animal studies and clinical studies in women, 19‐norderived progestins are known to be potent in terms of gonadotropin suppression (Couzinet et al, 1996). Among this class of steroidal compounds are norethisterone (NET), norethynodrel, and its dextrorotatory isomer LNG (ie, the biologically active form of this progestin). The progestins of this class are known to be potent suppressors of gonadotropin secretion, and when administered to men these compounds induced a profound suppression of sperm production (Frick, 1973). However, a decrease of libido and sexual potency was also reported, presumably due to the suppression of T production secondary to gonadotropin suppression (Kamischke et al, 2000b). Therefore, like other progestins available thus far, nor‐progestins should not be administered alone for male contraception because their residual androgenic activity is not sufficient to maintain androgen‐dependent physiological functions like libido or sexual potency (Kamischke et al, 2000a).
- S2CID 41502711.
- ^ PMID 7825629.
- ISBN 978-1-4612-4340-3. Archivedfrom the original on 8 September 2017.
- ISBN 978-1-60831-270-2. Archivedfrom the original on 8 September 2017.
- ISBN 9780309044936. NAP:13774. Archivedfrom the original on 8 September 2017.
- ^ S2CID 29808177.
- ^ S2CID 11302554.
- PMID 31512725.
- ^ ISBN 978-1-4757-2085-3. Archivedfrom the original on 8 September 2017.
- ^ ISBN 978-3-88763-075-1. Archivedfrom the original on 2017-09-08.
- ISBN 978-1-60913-713-7. Archivedfrom the original on 8 September 2017.
- ISBN 978-1-4612-5064-7. Archivedfrom the original on 8 September 2017.
- ISBN 978-3-540-38916-3. Archivedfrom the original on 8 September 2017.
- S2CID 32126275.
- ^ a b Population Reports: Injectables and implants. Department of Medical and Public Affairs, George Washington University. 1987. Archived from the original on 2021-04-20. Retrieved 2018-04-15.
The Population Council also plans to test vaginal rings with two other progestins, ST-1435 and levonorgestrel acetate, alone and combined with ethinyl estradiol (168).
- ^ S2CID 12896179.
- ^ "Levonorgestrel". PubChem. Retrieved 18 August 2022.
- ^ "Levonorgestrel: Uses, Interactions, Mechanism of Action". DrugBank Online. 30 October 2013. Retrieved 18 August 2022.
- ISBN 978-1-59259-700-0. Archivedfrom the original on 1 August 2020. Retrieved 15 April 2018.
The gonanes share the structural modifications found in the estranes and also possess [an ethyl] group at the position 13 and a keto group at position 3. Norgestrel was synthesized in 1963 and is a racemic mixture of dextro and levorotatory forms. The levorotatory form, levonorgestrel, provides the biological activity.
- ISBN 978-94-011-5448-2. Archivedfrom the original on 28 August 2021. Retrieved 15 April 2018.
[Norgestrel] was discovered by Hughes et al. (1963).
- ^ ISBN 978-1-4831-6366-6.
Norgestrel, developed by Wyeth and patented in 1964, was the first progestogen to be manufactured by total chemical synthesis. It was subsequently licensed to Schering AG, who separated the racemic mixture into an inactive structural isomer l-norgestrel and the active d-norgestrel -- more usually known as dextronorgestrel and levonorgestrel respectively, because of the optical isomerism that each displays.
- ^ ISBN 978-0-300-16791-7.
In 1964 the pharmaceutical company Wyeth developed norgestrel, the first progestogen to be made from a total chemical synthesis. Subsequently licensed to Schering AG, norgestrel was used to develop levonorgestrel, another active progestogen later used for oral contraception.
- ^ ISBN 978-3-205-77303-0. Archivedfrom the original on 2021-08-28. Retrieved 2018-04-18.
[The contraceptive EUGYNON is launched in 1966. NEOGYNON follows in 1970.]
- ^ ISBN 978-1-317-12981-3. Archivedfrom the original on 6 October 2021. Retrieved 18 April 2018.
The 1966 marketing campaign for Schering's second contraceptive, Eugynon, [...] (Schering AG Berline 1966, 11). [...] In 1970 [Schering] had already conducted an opinion poll among doctors in the run up to the marketing campaign for the newly introduced Neogynon. [...]
- ISBN 978-0-8147-8300-9.
- ISBN 978-3-11-013947-1. Archivedfrom the original on August 28, 2021. Retrieved August 5, 2020.
[Since the safety of ovulation inhibition by levonorgestrel was also proven in the clinical studies, the cycle was extremely stable and the side effects were low, the drug was on August 1, 1970 introduced as Neogynon 21 and Neogynon 28 in Germany on the market.] [...] After the OC market had risen sharply in 1968 and 1969, the launch of Neogynon / Schering and Stediril-d / Wyeth in August 1970 gave the market a fresh boost.]
- ISSN 0010-7824.
The results obtained in these series clinically confirmed the findings in animal work on the potency of d-norgestrel, i.e., that the biological activity of norgestrel resides largely in the d-enantlomer (5,6).
- ^ Brosens I, Van Assche A, Wijnants P (1971). "Comparative clinical and morphological studies on 2 oral contraceptives which contain DL-norgestrel and D-norgestrel respectively". Geburtshilfe und Frauenheilkunde. 31 (3): 251–257. Archived from the original on 2018-04-15. Retrieved 2018-04-15.
Comparison of the effects of Eugynon and Neogynon (.05 mg ethinyl estradiol with .5 mg norgestrel or with .25 mg d-norgestrel, respectively) in 272 women is reported. The 2 preparations were comparable as regards effectiveness (100%), cycle control, and endometrial and cervical morphology. No clinical or biological complications occurred, and the incidence of minor side effects was very small. The d-norgestrel preparation (Neogynon) may be preferable for metabolic reasons because of its lower steroid dose.
- ISSN 0010-7824.
- PMID 4614952.
- ^ a b Scharff HJ (1972). "Clinical experience with Microlut". Medical News Schering (1): 2–9. Archived from the original on 2018-04-15.
- from the original on 2018-04-15. Retrieved 2018-04-15.
- ^ ISSN 0010-7824.
- ISSN 0010-7824.
- ISBN 978-81-312-0300-2. Archivedfrom the original on 28 August 2021. Retrieved 15 April 2018.
There are two main methods involving oral emergency pills, commonly misleadingly described as the 'morning-after pill'. The first older method, developed in the mid-1970s, involves two high-dose combined pills containing oestrogen (50 ug ethinyloestradiol) and progesterone (0.25 mg levonorgestrel): the Yuzpe regime (Schering PC4 or Ovran). The second involves progesterone only (0.75 mg levonorgestrel), and therefore, has a lower incidence of side effects, in particular vomiting (6%).
- PMID 4844513.
- ^ Farkas M (1978). "Post-coital contraception with Postinor, a preparation containing 0.75 mg d-norgestrel". Magyar Nöorvosok Lapja. 41: 474.
- ISBN 978-1-84214-071-0. Archivedfrom the original on 28 August 2021. Retrieved 15 April 2018.
- PMID 8473453.
- ISBN 978-1-284-02542-2. Archivedfrom the original on 28 August 2021. Retrieved 15 April 2018.
- ISBN 978-3-319-12406-3. Archivedfrom the original on 28 August 2021. Retrieved 15 April 2018.
- ^ a b "FDA approves over-the-counter sales of Plan B One-Step for all ages". CBS News. 20 June 2013. Archived from the original on 2017-08-03. Retrieved 2017-08-03.
- ^ Trussell J, Cleland K (2007-04-10). "Emergency Contraceptive Pills Worldwide". Princeton University. Archived from the original on 2007-05-22. Retrieved 2007-05-28.
- ISBN 978-0-7234-3719-2.
- ISBN 978-0-674-01282-0.
- ^ Dugan Arnett (March 27, 2022). "As some states seek to limit reproductive freedoms, BU opens 'Plan B' vending machine". The Boston Globe. Archived from the original on March 28, 2022. Retrieved March 28, 2022.
- ^ Rankin K (2015-10-22). "This Policy Gives Native Women Equal Access to Emergency Contraception". Colorlines. Archived from the original on 2015-10-26. Retrieved 2015-10-24.
External links
![]() Media related to Levonorgestrel at Wikimedia Commons
Media related to Levonorgestrel at Wikimedia Commons
