Ethinylestradiol
Vaginal | |
| Drug class | Estrogen |
|---|---|
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 38–48%[2][3][4] |
| Protein binding | 97–98% (to albumin;[5] is not bound to SHBG)[6] |
| Metabolism | Liver (primarily CYP3A4)[9] |
| Metabolites | • Ethinylestradiol sulfate[7][8] • Others[7][8] |
| Elimination half-life | 7–36 hours[9][2][10][11] |
| Excretion | Feces: 62%[10] Urine: 38%[10] |
| Identifiers | |
| |
JSmol) | |
| Melting point | 182 to 184 °C (360 to 363 °F) |
| |
| |
| (verify) | |
Ethinylestradiol (EE) is an
The general
EE is an
EE was developed in the 1930s and was introduced for medical use in 1943.[13][14] The medication started being used in birth control pills in the 1960s.[15] Ethinylestradiol is found in almost all combined forms of birth control pills and is nearly the exclusive estrogen used for this purpose, making it one of the most widely used estrogens.[16][17]
In 2021, the combination with norethisterone was the 52nd most commonly prescribed medication in the United States, with more than 12 million prescriptions;[18][19] the version with norgestimate was the 76th most commonly prescribed medication in the US, with more than 8 million prescriptions;[18][20] the combination with levonorgestrel was the 144th most commonly prescribed medication in the US, with more than 4 million prescriptions;[18][21] the combination with etonogestrel was the 198th most commonly prescribed medication in the US, with more than 2 million prescriptions;[18][22] the combination with norgestrel was the 227th most commonly prescribed medication in the US, with more than 2 million prescriptions;[18][23] the combination with etynodiol was the 276th most commonly prescribed medication in the US, with more than 800,000 prescriptions;[18][24] the combination with drospirenone and levomefolic acid was the 277th most commonly prescribed medication in the US, with more than 800,000 prescriptions;[18][25]
Medical uses
There are many uses for EE. It is most commonly used as
EE is also used as
EE can also be used to treat
EE or any estrogen alone is contraindicated for women who have a uterus due to the increased risk of endometrial cancer; giving a progestogen with an estrogen mitigates the risk.[32]
Available forms
EE is available in combination with a progestin in a vast number of COCs.
The amount of EE in COCs has reduced over the years.[8] Previously, COCs contained high doses of EE of as much as 100 µg/day.[39] Doses of more than 50 µg EE are considered high-dose, doses of 30 and 35 µg EE are considered low-dose, and doses of 10 to 25 µg EE are considered very low dose.[40] Today, COCs generally contain 10 to 50 µg EE.[40] The higher doses of EE were discontinued due to a high risk of VTE and cardiovascular problems.[39]
Contraindications
EE should be avoided in individuals with a history of or known susceptibility to
- History of anticoagulants
- Acute DVT/PE
- Prolonged immobilization due to major surgery
- Advanced diabetes mellituswith vascular disease
- Migraine with aura
- Hypertension ≥160/100
- Vascular disease
- Current and history of ischemic heart disease
- Multiple risk factors for atherosclerotic cardiovascular disease(e.g. older age, smoking, diabetes, hypertension, low HDL, high LDL, or high triglyceride levels)
- Age ≥35 and smoking ≥15 cigarettes/day
- History of cerebrovascular accident
- Systemic lupus erythematosus with positive (or unknown) antiphospholipid antibodies
- Complicated valvular heart disease
Except when being used to treat it, EE should be avoided in women with current breast cancer due to a possible worsening of prognosis.[42]
EE should also be avoided in
Due to risk of
Side effects
| Ethinylestradiol dose | No. of VTE cases | Woman-years | VTE rate | Adjusted RRa |
|---|---|---|---|---|
| Low (<50 μg) | 53 | 127,000 | 4.2 in 10,000 woman-years | 1.0 |
| Intermediate (50 μg) | 69 | 98,000 | 7.0 in 10,000 woman-years | 1.5 |
| High (>50 μg) | 20 | 20,000 | 10.0 in 10,000 woman-years | 1.7 |
| All | 142 | 245,000 | 5.8 in 10,000 woman-years | – |
| Footnotes: a = Relative to low-dose (not to non-use). Notes: In birth control pills containing a first-generation progestin, such as norethisterone or levonorgestrel. Sources: Main:[45][46] Additional:[47]
| ||||
The severity of side effects can vary based on the dose and administration route of EE.
Long-term effects
| Beneficial effects | Adverse effects | ||
|---|---|---|---|
| Disease | RR | Disease | RR |
| Iron-deficiency anemia | 0.58 | Cardiovascular diseases (total) | 1.5 |
Menorrhagia |
0.52 | Myocardial infarction (heart attack) (total) | 3.3 |
| Irregular menstruation | 0.65 | Myocardial infarction (non-smokers) | 1.0 |
Intermenstrual bleeding |
0.72 | Myocardial infarction (light smokers) | 3.5 |
| Dysmenorrhea | 0.37 | Myocardial infarction (heavy smokers) | 20 |
| Pelvic inflammatory disease (incidence) | 0.50 | Cerebrovascular diseases (total) | 1.4 |
hospitalization ) |
0.22 | Cerebral thromboses (strokes) |
2.5 |
Trichomonas vaginitis |
0.56 | Subarachnoidal bleeding (heavy smokers ) |
10 |
Benign breast disease |
0.69 | Pulmonary embolism | 3.0 |
Fibrocystic breast disease |
0.66 | Deep vein thromboses | 2.5 |
Benign breast fibroadenomas |
0.35 | Gall-bladder diseases |
3.0 |
| Rheumatoid arthritis | 0.49 | Benign liver tumors |
50 |
| Endometrial cancer | 0.40–0.50 | Hepatocellular carcinoma | 3.0 |
| Ovarian cancer (incidence) | 0.37–0.64 | Erythema nodosum et multiforme | 3.0 |
| Ovarian cancer (death) | 0.20 | Pruritus (itching) |
2.0 |
| Benign follicular cysts (high-dose COCs) | 0.24 | Photosensitive eczema |
4.0 |
Acne vulgaris |
0.44 | Irritant agent eczema |
2.0 |
Low bone mineral density (later in life) |
0.35a | Dermatitis (eczema) | 2.0 |
| Ectopic pregnancy | 0.19 | Chloasma (melasma) |
1.5 |
| Cervicitis (6 years of use) | 3.0 | ||
Chlamydia infections |
2.5 | ||
| Footnotes: a = Odds ratio. Sources: [50][34] | |||
Blood clots
VTE is a
A 2012
Modern COCs contain 10 to 35 μg EE, but typically 20, 30, or 35 μg.
Women with thrombophilia have a dramatically higher risk of VTE with EE-containing contraception than women without thrombophilia.[53][54] Depending on the condition, risk of VTE can be increased 5- to 50-fold relative to non-use in such women.[53][54]
| Type | Route | Medications | Odds ratio (95% CI) |
|---|---|---|---|
Menopausal hormone therapy |
Oral | Estradiol alone ≤1 mg/day >1 mg/day |
1.27 (1.16–1.39)* 1.22 (1.09–1.37)* 1.35 (1.18–1.55)* |
| Conjugated estrogens alone ≤0.625 mg/day >0.625 mg/day |
1.49 (1.39–1.60)* 1.40 (1.28–1.53)* 1.71 (1.51–1.93)* | ||
| Estradiol/medroxyprogesterone acetate | 1.44 (1.09–1.89)* | ||
| Estradiol/dydrogesterone ≤1 mg/day E2 >1 mg/day E2 |
1.18 (0.98–1.42) 1.12 (0.90–1.40) 1.34 (0.94–1.90) | ||
| Estradiol/norethisterone ≤1 mg/day E2 >1 mg/day E2 |
1.68 (1.57–1.80)* 1.38 (1.23–1.56)* 1.84 (1.69–2.00)* | ||
Estradiol/norgestrel or estradiol/drospirenone |
1.42 (1.00–2.03) | ||
| Conjugated estrogens/medroxyprogesterone acetate | 2.10 (1.92–2.31)* | ||
| Conjugated estrogens/norgestrel ≤0.625 mg/day CEEs >0.625 mg/day CEEs |
1.73 (1.57–1.91)* 1.53 (1.36–1.72)* 2.38 (1.99–2.85)* | ||
| Tibolone alone | 1.02 (0.90–1.15) | ||
| Raloxifene alone | 1.49 (1.24–1.79)* | ||
Transdermal |
Estradiol alone ≤50 μg/day >50 μg/day |
0.96 (0.88–1.04) 0.94 (0.85–1.03) 1.05 (0.88–1.24) | |
| Estradiol/progestogen | 0.88 (0.73–1.01) | ||
Vaginal |
Estradiol alone | 0.84 (0.73–0.97) | |
| Conjugated estrogens alone | 1.04 (0.76–1.43) | ||
Combined birth control |
Oral | Ethinylestradiol/norethisterone | 2.56 (2.15–3.06)* |
| Ethinylestradiol/levonorgestrel | 2.38 (2.18–2.59)* | ||
Ethinylestradiol/norgestimate |
2.53 (2.17–2.96)* | ||
| Ethinylestradiol/desogestrel | 4.28 (3.66–5.01)* | ||
| Ethinylestradiol/gestodene | 3.64 (3.00–4.43)* | ||
| Ethinylestradiol/drospirenone | 4.12 (3.43–4.96)* | ||
| Ethinylestradiol/cyproterone acetate | 4.27 (3.57–5.11)* | ||
| Notes: (1) Bioidentical progesterone was not included, but is known to be associated with no additional risk relative to estrogen alone. Footnotes: * = Statistically significant (p < 0.01). Sources: See template.
| |||
Cardiovascular issues
When used orally at high dosages, for instance as a form of high-dose estrogen therapy in men with prostate cancer and in women with breast cancer,
In contrast to oral synthetic estrogens like EE and diethylstilbestrol, high-dosage
Because of its disproportionate effects on liver protein synthesis and associated cardiovascular risks, synthetic estrogens like EE and diethylstilbestrol are no longer used in menopausal hormone therapy.[8] They are also being replaced by parenteral forms of estradiol like polyestradiol phosphate and transdermal estradiol in the treatment of prostate cancer.[73]
Liver damage
At the lower dosages that are now used in birth control pills, EE has been associated rarely with
Uterine cancer
The high doses of EE that were used in early COCs were associated with a significantly increased risk of endometrial cancer in certain preparations, for instance those containing the progestogen dimethisterone.[85] Unopposed estrogens like EE have carcinogenic effects in the endometrium and progestogens protect against these effects, but dimethisterone is a relatively weak progestogen and was unable to adequately antagonize the endometrial carcinogenic effects of EE, in turn resulting in the increased risk of endometrial cancer.[85] COCs containing dimethisterone have since been discontinued (with more potent progestogens used instead) and doses of EE in COCs in general have been dramatically reduced, abrogating the risk.[85] In turn, most studies of modern COCs have found a decreased risk of endometrial cancer.[86]
Ecological Effects
Wastewater contains various estrogens, including EE, that are not completely broken down by wastewater treatment procedures.[87] The input of artificial estrogens into freshwater ecosystems affects fish and amphibian populations. Chronic exposure to low levels of EE over seven years led to the collapse of fathead minnow populations in an experimental lake in Ontario, Canada.[87] EE changed oogenesis in female fish and feminized male fish such that they produced a protein associated with egg maturation, vitellogenin, as well as early-stage eggs.[87] In amphibians, exposure to EE can reduce hatching success and alter gonadal development.[88] Exposure to hormones can change frogs' gonadal development even though it is encoded in their genes.[88] A study of mink frogs found more intersex tadpoles in those experimentally exposed to EE than those not exposed to EE, and green frogs showed much lower rates of hatching success.[88]
Overdose
Estrogens like EE are relatively safe in acute
Interactions
EE is metabolized by certain
In contrast to estradiol, it is unlikely that there is a pharmacokinetic interaction between smoking (which potently induces certain cytochrome P450 enzymes and markedly increases the 2-hydroxylation of estradiol) and EE.[44] This suggests that estradiol and EE are metabolized by different cytochrome P450 enzymes.[44] There is, however, an increased risk of cardiovascular complications with smoking and EE, similarly to the case of smoking and other estrogens.[44]
EE is known to inhibit several cytochrome P450 enzymes, including CYP1A2, CYP2B6, CYP2C9, CYP2C19, and CYP3A4, and is possibly an inducer of CYP2A6.[90] As a result, it can affect the metabolism and concentrations of many other drugs.[90] Examples of known interactions include bupropion, caffeine, mephenytoin, midazolam, nicotine, nifedipine, omeprazole, propranolol, proguanil, selegiline, theophylline, and tizanidine.[90][44] One of the most notable interactions is that EE strongly increases levels of selegiline, a substrate of CYP2B6 and CYP2C19.[90] EE may also induce glucuronidation and possibly alter sulfation.[90] It has been found to increase the clearance of and reduce the concentrations of a variety of drugs known to be glucuronidated.[90] Examples include clofibrate, lamotrigine, lorazepam, oxazepam, and propranolol.[90]
Progestins, which are often used in combination with EE, are also known to inhibit cytochrome P450 enzymes, and this may contribute to drug interactions with EE-containing contraceptives as well.[90] Examples include gestodene, desogestrel, and etonogestrel, which are CYP3A4 and CYP2C19 inhibitors.[90] In addition, these progestins are known to progressively inhibit the metabolism of and increase concentrations of EE itself.[44]
Pharmacology
Pharmacodynamics
EE is an
EE is a long-acting estrogen, with a nuclear retention of about 24 hours.[46]
Orally, EE is on the order of 100 times as potent by weight as natural estrogens like
| Ligand | Other names | Relative binding affinities (RBA, %)a |
Absolute binding affinities (Ki, nM)a |
Action | ||
|---|---|---|---|---|---|---|
ERα |
ERβ |
ERα |
ERβ
| |||
| Estradiol | E2; 17β-Estradiol | 100 | 100 | 0.115 (0.04–0.24) | 0.15 (0.10–2.08) | Estrogen |
| Estrone | E1; 17-Ketoestradiol | 16.39 (0.7–60) | 6.5 (1.36–52) | 0.445 (0.3–1.01) | 1.75 (0.35–9.24) | Estrogen |
| Estriol | E3; 16α-OH-17β-E2 | 12.65 (4.03–56) | 26 (14.0–44.6) | 0.45 (0.35–1.4) | 0.7 (0.63–0.7) | Estrogen |
| Estetrol | E4; 15α,16α-Di-OH-17β-E2 | 4.0 | 3.0 | 4.9 | 19 | Estrogen |
| Alfatradiol | 17α-Estradiol | 20.5 (7–80.1) | 8.195 (2–42) | 0.2–0.52 | 0.43–1.2 | Metabolite |
16-Epiestriol |
16β-Hydroxy-17β-estradiol | 7.795 (4.94–63) | 50 | ? | ? | Metabolite |
17-Epiestriol |
16α-Hydroxy-17α-estradiol | 55.45 (29–103) | 79–80 | ? | ? | Metabolite |
16,17-Epiestriol |
16β-Hydroxy-17α-estradiol | 1.0 | 13 | ? | ? | Metabolite |
| 2-Hydroxyestradiol | 2-OH-E2 | 22 (7–81) | 11–35 | 2.5 | 1.3 | Metabolite |
| 2-Methoxyestradiol | 2-MeO-E2 | 0.0027–2.0 | 1.0 | ? | ? | Metabolite |
| 4-Hydroxyestradiol | 4-OH-E2 | 13 (8–70) | 7–56 | 1.0 | 1.9 | Metabolite |
| 4-Methoxyestradiol | 4-MeO-E2 | 2.0 | 1.0 | ? | ? | Metabolite |
| 2-Hydroxyestrone | 2-OH-E1 | 2.0–4.0 | 0.2–0.4 | ? | ? | Metabolite |
| 2-Methoxyestrone | 2-MeO-E1 | <0.001–<1 | <1 | ? | ? | Metabolite |
| 4-Hydroxyestrone | 4-OH-E1 | 1.0–2.0 | 1.0 | ? | ? | Metabolite |
| 4-Methoxyestrone | 4-MeO-E1 | <1 | <1 | ? | ? | Metabolite |
| 16α-Hydroxyestrone | 16α-OH-E1; 17-Ketoestriol | 2.0–6.5 | 35 | ? | ? | Metabolite |
| 2-Hydroxyestriol | 2-OH-E3 | 2.0 | 1.0 | ? | ? | Metabolite |
| 4-Methoxyestriol | 4-MeO-E3 | 1.0 | 1.0 | ? | ? | Metabolite |
| Estradiol sulfate | E2S; Estradiol 3-sulfate | <1 | <1 | ? | ? | Metabolite |
| Estradiol disulfate | Estradiol 3,17β-disulfate | 0.0004 | ? | ? | ? | Metabolite |
| Estradiol 3-glucuronide | E2-3G | 0.0079 | ? | ? | ? | Metabolite |
Estradiol 17β-glucuronide |
E2-17G | 0.0015 | ? | ? | ? | Metabolite |
| Estradiol 3-gluc. 17β-sulfate | E2-3G-17S | 0.0001 | ? | ? | ? | Metabolite |
| Estrone sulfate | E1S; Estrone 3-sulfate | <1 | <1 | >10 | >10 | Metabolite |
| Estradiol benzoate | EB; Estradiol 3-benzoate | 10 | ? | ? | ? | Estrogen |
| Estradiol 17β-benzoate | E2-17B | 11.3 | 32.6 | ? | ? | Estrogen |
| Estrone methyl ether | Estrone 3-methyl ether | 0.145 | ? | ? | ? | Estrogen |
| ent-Estradiol | 1-Estradiol | 1.31–12.34 | 9.44–80.07 | ? | ? | Estrogen |
| Equilin | 7-Dehydroestrone | 13 (4.0–28.9) | 13.0–49 | 0.79 | 0.36 | Estrogen |
| Equilenin | 6,8-Didehydroestrone | 2.0–15 | 7.0–20 | 0.64 | 0.62 | Estrogen |
| 17β-Dihydroequilin | 7-Dehydro-17β-estradiol | 7.9–113 | 7.9–108 | 0.09 | 0.17 | Estrogen |
| 17α-Dihydroequilin | 7-Dehydro-17α-estradiol | 18.6 (18–41) | 14–32 | 0.24 | 0.57 | Estrogen |
| 17β-Dihydroequilenin | 6,8-Didehydro-17β-estradiol | 35–68 | 90–100 | 0.15 | 0.20 | Estrogen |
| 17α-Dihydroequilenin | 6,8-Didehydro-17α-estradiol | 20 | 49 | 0.50 | 0.37 | Estrogen |
| Δ8-Estradiol | 8,9-Dehydro-17β-estradiol | 68 | 72 | 0.15 | 0.25 | Estrogen |
| Δ8-Estrone | 8,9-Dehydroestrone | 19 | 32 | 0.52 | 0.57 | Estrogen |
| Ethinylestradiol | EE; 17α-Ethynyl-17β-E2 | 120.9 (68.8–480) | 44.4 (2.0–144) | 0.02–0.05 | 0.29–0.81 | Estrogen |
| Mestranol | EE 3-methyl ether | ? | 2.5 | ? | ? | Estrogen |
| Moxestrol | RU-2858; 11β-Methoxy-EE | 35–43 | 5–20 | 0.5 | 2.6 | Estrogen |
| Methylestradiol | 17α-Methyl-17β-estradiol | 70 | 44 | ? | ? | Estrogen |
| Diethylstilbestrol | DES; Stilbestrol | 129.5 (89.1–468) | 219.63 (61.2–295) | 0.04 | 0.05 | Estrogen |
| Hexestrol | Dihydrodiethylstilbestrol | 153.6 (31–302) | 60–234 | 0.06 | 0.06 | Estrogen |
| Dienestrol | Dehydrostilbestrol | 37 (20.4–223) | 56–404 | 0.05 | 0.03 | Estrogen |
| Benzestrol (B2) | – | 114 | ? | ? | ? | Estrogen |
| Chlorotrianisene | TACE | 1.74 | ? | 15.30 | ? | Estrogen |
| Triphenylethylene | TPE | 0.074 | ? | ? | ? | Estrogen |
| Triphenylbromoethylene | TPBE | 2.69 | ? | ? | ? | Estrogen |
| Tamoxifen | ICI-46,474 | 3 (0.1–47) | 3.33 (0.28–6) | 3.4–9.69 | 2.5 | SERM |
| Afimoxifene | 4-Hydroxytamoxifen; 4-OHT | 100.1 (1.7–257) | 10 (0.98–339) | 2.3 (0.1–3.61) | 0.04–4.8 | SERM |
| Toremifene | 4-Chlorotamoxifen; 4-CT | ? | ? | 7.14–20.3 | 15.4 | SERM |
| Clomifene | MRL-41 | 25 (19.2–37.2) | 12 | 0.9 | 1.2 | SERM |
| Cyclofenil | F-6066; Sexovid | 151–152 | 243 | ? | ? | SERM |
| Nafoxidine | U-11,000A | 30.9–44 | 16 | 0.3 | 0.8 | SERM |
| Raloxifene | – | 41.2 (7.8–69) | 5.34 (0.54–16) | 0.188–0.52 | 20.2 | SERM |
| Arzoxifene | LY-353,381 | ? | ? | 0.179 | ? | SERM |
| Lasofoxifene | CP-336,156 | 10.2–166 | 19.0 | 0.229 | ? | SERM |
| Ormeloxifene | Centchroman | ? | ? | 0.313 | ? | SERM |
| Levormeloxifene | 6720-CDRI; NNC-460,020 | 1.55 | 1.88 | ? | ? | SERM |
| Ospemifene | Deaminohydroxytoremifene | 0.82–2.63 | 0.59–1.22 | ? | ? | SERM |
| Bazedoxifene | – | ? | ? | 0.053 | ? | SERM |
| Etacstil | GW-5638 | 4.30 | 11.5 | ? | ? | SERM |
ICI-164,384 |
– | 63.5 (3.70–97.7) | 166 | 0.2 | 0.08 | Antiestrogen |
| Fulvestrant | ICI-182,780 | 43.5 (9.4–325) | 21.65 (2.05–40.5) | 0.42 | 1.3 | Antiestrogen |
| Propylpyrazoletriol | PPT | 49 (10.0–89.1) | 0.12 | 0.40 | 92.8 | ERα agonist |
| 16α-LE2 | 16α-Lactone-17β-estradiol | 14.6–57 | 0.089 | 0.27 | 131 | ERα agonist |
| 16α-Iodo-E2 | 16α-Iodo-17β-estradiol | 30.2 | 2.30 | ? | ? | ERα agonist |
| Methylpiperidinopyrazole | MPP | 11 | 0.05 | ? | ? | ERα antagonist |
| Diarylpropionitrile | DPN | 0.12–0.25 | 6.6–18 | 32.4 | 1.7 | ERβ agonist |
| 8β-VE2 | 8β-Vinyl-17β-estradiol | 0.35 | 22.0–83 | 12.9 | 0.50 | ERβ agonist |
| Prinaberel | ERB-041; WAY-202,041 | 0.27 | 67–72 | ? | ? | ERβ agonist |
| ERB-196 | WAY-202,196 | ? | 180 | ? | ? | ERβ agonist |
| Erteberel | SERBA-1; LY-500,307 | ? | ? | 2.68 | 0.19 | ERβ agonist |
| SERBA-2 | – | ? | ? | 14.5 | 1.54 | ERβ agonist |
| Coumestrol | – | 9.225 (0.0117–94) | 64.125 (0.41–185) | 0.14–80.0 | 0.07–27.0 | Xenoestrogen |
| Genistein | – | 0.445 (0.0012–16) | 33.42 (0.86–87) | 2.6–126 | 0.3–12.8 | Xenoestrogen |
| Equol | – | 0.2–0.287 | 0.85 (0.10–2.85) | ? | ? | Xenoestrogen |
| Daidzein | – | 0.07 (0.0018–9.3) | 0.7865 (0.04–17.1) | 2.0 | 85.3 | Xenoestrogen |
| Biochanin A | – | 0.04 (0.022–0.15) | 0.6225 (0.010–1.2) | 174 | 8.9 | Xenoestrogen |
| Kaempferol | – | 0.07 (0.029–0.10) | 2.2 (0.002–3.00) | ? | ? | Xenoestrogen |
| Naringenin | – | 0.0054 (<0.001–0.01) | 0.15 (0.11–0.33) | ? | ? | Xenoestrogen |
| 8-Prenylnaringenin | 8-PN | 4.4 | ? | ? | ? | Xenoestrogen |
| Quercetin | – | <0.001–0.01 | 0.002–0.040 | ? | ? | Xenoestrogen |
| Ipriflavone | – | <0.01 | <0.01 | ? | ? | Xenoestrogen |
| Miroestrol | – | 0.39 | ? | ? | ? | Xenoestrogen |
Deoxymiroestrol |
– | 2.0 | ? | ? | ? | Xenoestrogen |
β-Sitosterol |
– | <0.001–0.0875 | <0.001–0.016 | ? | ? | Xenoestrogen |
| Resveratrol | – | <0.001–0.0032 | ? | ? | ? | Xenoestrogen |
| α-Zearalenol | – | 48 (13–52.5) | ? | ? | ? | Xenoestrogen |
| β-Zearalenol | – | 0.6 (0.032–13) | ? | ? | ? | Xenoestrogen |
| Zeranol | α-Zearalanol | 48–111 | ? | ? | ? | Xenoestrogen |
| Taleranol | β-Zearalanol | 16 (13–17.8) | 14 | 0.8 | 0.9 | Xenoestrogen |
| Zearalenone | ZEN | 7.68 (2.04–28) | 9.45 (2.43–31.5) | ? | ? | Xenoestrogen |
| Zearalanone | ZAN | 0.51 | ? | ? | ? | Xenoestrogen |
| Bisphenol A | BPA | 0.0315 (0.008–1.0) | 0.135 (0.002–4.23) | 195 | 35 | Xenoestrogen |
| Endosulfan | EDS | <0.001–<0.01 | <0.01 | ? | ? | Xenoestrogen |
Kepone |
Chlordecone | 0.0069–0.2 | ? | ? | ? | Xenoestrogen |
o,p'-DDT |
– | 0.0073–0.4 | ? | ? | ? | Xenoestrogen |
p,p'-DDT |
– | 0.03 | ? | ? | ? | Xenoestrogen |
| Methoxychlor | p,p'-Dimethoxy-DDT | 0.01 (<0.001–0.02) | 0.01–0.13 | ? | ? | Xenoestrogen |
| HPTE | Hydroxychlor; p,p'-OH-DDT | 1.2–1.7 | ? | ? | ? | Xenoestrogen |
| Testosterone | T; 4-Androstenolone | <0.0001–<0.01 | <0.002–0.040 | >5000 | >5000 | Androgen |
| Dihydrotestosterone | DHT; 5α-Androstanolone | 0.01 (<0.001–0.05) | 0.0059–0.17 | 221–>5000 | 73–1688 | Androgen |
| Nandrolone | 19-Nortestosterone; 19-NT | 0.01 | 0.23 | 765 | 53 | Androgen |
| Dehydroepiandrosterone | DHEA; Prasterone | 0.038 (<0.001–0.04) | 0.019–0.07 | 245–1053 | 163–515 | Androgen |
5-Androstenediol |
A5; Androstenediol | 6 | 17 | 3.6 | 0.9 | Androgen |
| 4-Androstenediol | – | 0.5 | 0.6 | 23 | 19 | Androgen |
4-Androstenedione |
A4; Androstenedione | <0.01 | <0.01 | >10000 | >10000 | Androgen |
| 3α-Androstanediol | 3α-Adiol | 0.07 | 0.3 | 260 | 48 | Androgen |
| 3β-Androstanediol | 3β-Adiol | 3 | 7 | 6 | 2 | Androgen |
| Androstanedione | 5α-Androstanedione | <0.01 | <0.01 | >10000 | >10000 | Androgen |
| Etiocholanedione | 5β-Androstanedione | <0.01 | <0.01 | >10000 | >10000 | Androgen |
| Methyltestosterone | 17α-Methyltestosterone | <0.0001 | ? | ? | ? | Androgen |
Ethinyl-3α-androstanediol |
17α-Ethynyl-3α-adiol | 4.0 | <0.07 | ? | ? | Estrogen |
Ethinyl-3β-androstanediol |
17α-Ethynyl-3β-adiol | 50 | 5.6 | ? | ? | Estrogen |
| Progesterone | P4; 4-Pregnenedione | <0.001–0.6 | <0.001–0.010 | ? | ? | Progestogen |
| Norethisterone | NET; 17α-Ethynyl-19-NT | 0.085 (0.0015–<0.1) | 0.1 (0.01–0.3) | 152 | 1084 | Progestogen |
Norethynodrel |
5(10)-Norethisterone | 0.5 (0.3–0.7) | <0.1–0.22 | 14 | 53 | Progestogen |
| Tibolone | 7α-Methylnorethynodrel | 0.5 (0.45–2.0) | 0.2–0.076 | ? | ? | Progestogen |
| Δ4-Tibolone | 7α-Methylnorethisterone | 0.069–<0.1 | 0.027–<0.1 | ? | ? | Progestogen |
| 3α-Hydroxytibolone | – | 2.5 (1.06–5.0) | 0.6–0.8 | ? | ? | Progestogen |
| 3β-Hydroxytibolone | – | 1.6 (0.75–1.9) | 0.070–0.1 | ? | ? | Progestogen |
| Footnotes: a = (1) ERβ proteins (except the ERβ values from Kuiper et al. (1997), which are rat ERβ). Sources: See template page.
| ||||||
| Estrogen | Relative binding affinities (%)
| ||||||
|---|---|---|---|---|---|---|---|
| ER | AR | PR | GR | MR | SHBG | CBG
| |
| Estradiol | 100 | 7.9 | 2.6 | 0.6 | 0.13 | 8.7–12 | <0.1 |
| Estradiol benzoate | ? | ? | ? | ? | ? | <0.1–0.16 | <0.1 |
| Estradiol valerate | 2 | ? | ? | ? | ? | ? | ? |
| Estrone | 11–35 | <1 | <1 | <1 | <1 | 2.7 | <0.1 |
| Estrone sulfate | 2 | 2 | ? | ? | ? | ? | ? |
| Estriol | 10–15 | <1 | <1 | <1 | <1 | <0.1 | <0.1 |
| Equilin | 40 | ? | ? | ? | ? | ? | 0 |
| Alfatradiol | 15 | <1 | <1 | <1 | <1 | ? | ? |
| Epiestriol | 20 | <1 | <1 | <1 | <1 | ? | ? |
| Ethinylestradiol | 100–112 | 1–3 | 15–25 | 1–3 | <1 | 0.18 | <0.1 |
| Mestranol | 1 | ? | ? | ? | ? | <0.1 | <0.1 |
| Methylestradiol | 67 | 1–3 | 3–25 | 1–3 | <1 | ? | ? |
| Moxestrol | 12 | <0.1 | 0.8 | 3.2 | <0.1 | <0.2 | <0.1 |
| Diethylstilbestrol | ? | ? | ? | ? | ? | <0.1 | <0.1 |
| Notes: Reference CBG . Sources: See template.
| |||||||
| Estrogen | HF |
VE | UCa | FSH | LH | HDL-C | SHBG | CBG |
AGT |
Liver |
|---|---|---|---|---|---|---|---|---|---|---|
| Estradiol | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Estrone | ? | ? | ? | 0.3 | 0.3 | ? | ? | ? | ? | ? |
| Estriol | 0.3 | 0.3 | 0.1 | 0.3 | 0.3 | 0.2 | ? | ? | ? | 0.67 |
| Estrone sulfate | ? | 0.9 | 0.9 | 0.8–0.9 | 0.9 | 0.5 | 0.9 | 0.5–0.7 | 1.4–1.5 | 0.56–1.7 |
| Conjugated estrogens | 1.2 | 1.5 | 2.0 | 1.1–1.3 | 1.0 | 1.5 | 3.0–3.2 | 1.3–1.5 | 5.0 | 1.3–4.5 |
Equilin sulfate |
? | ? | 1.0 | ? | ? | 6.0 | 7.5 | 6.0 | 7.5 | ? |
| Ethinylestradiol | 120 | 150 | 400 | 60–150 | 100 | 400 | 500–600 | 500–600 | 350 | 2.9–5.0 |
| Diethylstilbestrol | ? | ? | ? | 2.9–3.4 | ? | ? | 26–28 | 25–37 | 20 | 5.7–7.5 |
Sources and footnotes
Notes: Values are ratios, with estradiol as standard (i.e., 1.0). Abbreviations: HF = Clinical relief of liver proteins. Liver = Ratio of liver estrogenic effects to general/systemic estrogenic effects (hot flashes/gonadotropins ). Sources: See template. | ||||||||||
| Compound | Dosage for specific uses (mg usually)[a] | ||||||
|---|---|---|---|---|---|---|---|
| ETD[b] | EPD[b] | MSD[b] | MSD[c] | OID[c] | TSD[c] | ||
| Estradiol (non-micronized) | 30 | ≥120–300 | 120 | 6 | - | - | |
| Estradiol (micronized) | 6–12 | 60–80 | 14–42 | 1–2 | >5 | >8 | |
| Estradiol valerate | 6–12 | 60–80 | 14–42 | 1–2 | - | >8 | |
| Estradiol benzoate | - | 60–140 | - | - | - | - | |
| Estriol | ≥20 | 120–150[d] | 28–126 | 1–6 | >5 | - | |
| Estriol succinate | - | 140–150[d] | 28–126 | 2–6 | - | - | |
| Estrone sulfate | 12 | 60 | 42 | 2 | - | - | |
| Conjugated estrogens | 5–12 | 60–80 | 8.4–25 | 0.625–1.25 | >3.75 | 7.5 | |
| Ethinylestradiol | 200 μg | 1–2 | 280 μg | 20–40 μg | 100 μg | 100 μg | |
| Mestranol | 300 μg | 1.5–3.0 | 300–600 μg | 25–30 μg | >80 μg | - | |
| Quinestrol | 300 μg | 2–4 | 500 μg | 25–50 μg | - | - | |
| Methylestradiol | - | 2 | - | - | - | - | |
| Diethylstilbestrol | 2.5 | 20–30 | 11 | 0.5–2.0 | >5 | 3 | |
| DES dipropionate | - | 15–30 | - | - | - | - | |
| Dienestrol | 5 | 30–40 | 42 | 0.5–4.0 | - | - | |
| Dienestrol diacetate | 3–5 | 30–60 | - | - | - | - | |
| Hexestrol | - | 70–110 | - | - | - | - | |
| Chlorotrianisene | - | >100 | - | - | >48 | - | |
| Methallenestril | - | 400 | - | - | - | - | |
Sources and footnotes: | |||||||
Antiandrogenic and antigonadotropic effects
EE is a potent functional antiandrogen in both women and men.[125] It mediates its antiandrogenic effects by 1) stimulating the production of sex hormone-binding globulin (SHBG) in the liver, which decreases free and thus bioactive concentrations of testosterone in the blood; and by 2) suppressing luteinizing hormone (LH) secretion from the pituitary gland, which decreases production of testosterone by the gonads.[125][126][33][127] Birth control pills that contain EE are useful in the treatment of androgen-dependent conditions like acne and hirsutism by virtue of their antiandrogenic effects.[125][128]
Birth control pills containing EE have been found in women to reduce total testosterone levels by 30% on average, to increase circulating SHBG levels by about 3-fold on average (but variable depending on progestin, range 1.5- to 5-fold increase), and to reduce free testosterone concentrations by 60% on average (range 40 to 80%).[129][63][130][33] Birth control pills containing high doses of EE can increase SHBG levels in women by as much as 5- to 10-fold.[66] This is similar to the 5- to 10-fold increase in SHBG levels that occurs during pregnancy.[66] Due to the marked increase in SHBG levels, free testosterone levels become very low during treatment with EE-containing birth control pills.[10] In men, a study found that treatment with a relatively low dosage of 20 μg/day EE for five weeks increased circulating SHBG levels by 150% and, due to the accompanying decrease in free testosterone levels, increased total circulating levels of testosterone by 50% (via upregulation of gonadal testosterone production due to reduced negative feedback by androgens on the hypothalamic–pituitary–gonadal axis).[126] The stimulation of hepatic SHBG production by EE is far stronger than with other estrogens like estradiol, owing to the high resistance of EE to inactivation in the liver and hence its disproportionate effects in this part of the body.[7][10][131]
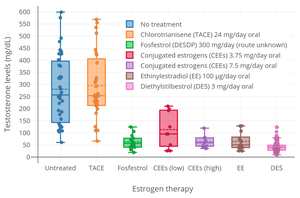
Estrogens are
Lower dosages of EE also have significant antigonadotropic effects.[135] A "very low" dosage of 15 µg/day EE has been described as the "borderline" amount required for suppression of LH and testosterone levels in men, and a study found that LH and testosterone levels were "reliably" suppressed in men by a dosage of 30 µg/day EE.[8] However, other clinical studies have found that 20 µg/day EE increased testosterone levels by 50% in men (as described above)[126] and that dosages of 32 µg/day and 42 µg/day EE suppressed FSH levels in men but did not significantly affect LH levels.[8] A stronger suppression of testosterone levels was observed in men following daily treatment with a combined oral contraceptive containing 50 µg ethinylestradiol and 0.5 mg norgestrel for 9 days.[8] However, investigation revealed that the progestin was the more important component responsible for the suppression in testosterone levels.[8] In accordance, the progestin component of COCs is primarily responsible for inhibition of ovulation in women.[8] A combination of 20 µg/day EE and 10 mg/day methyltestosterone was found to suppress FSH secretion in men to an extent sufficient to stop spermatogenesis.[8] Studies in women have found that 50 µg/day EE suppresses LH and FSH levels both by about 70% in postmenopausal women.[104]
In addition to its antigonadotropic effects, EE can significantly suppress androgen production by the
Effects on liver protein synthesis
EE has marked effects on
EE at 5 μg/day has been found to increase SHBG levels by 100% in postmenopausal women, while a dosage of 20 µg/day EE increased them by 200%.
A dosage of 10 µg/day EE has been found to increase CBG levels by 50%, while a dosage of 20 µg/day EE increased them by 100%.
Differences from estradiol


EE shows strong and disproportionate effects on
On the other hand, due to the loss of inactivation of EE by 17β-HSD in the endometrium (uterus), EE is relatively more active than estradiol in the endometrium and, for this reason, is associated with a significantly lower incidence of vaginal bleeding and spotting in comparison.[7] This is particularly so in the case of combined estrogen and progestogen therapy (as in COCs or menopausal HRT), as progestogens induce the expression of 17β-HSD in the endometrium.[7] The reduced vaginal bleeding and spotting with EE is one of the main reasons that it is used in COCs instead of estradiol,[3] in spite of its potentially inferior safety profile (related to its adverse effects on hepatic protein synthesis and VTE incidence).[150]
EE has been found to have disproportionate effects on liver protein synthesis and VTE risk regardless of whether the
| Parameters | Estradiol | Ethinylestradiol |
|---|---|---|
affinity |
1 × 1010 M-1 | 2–5 × 1011 M-1 |
| Nuclear retention | 6–8 hours | 24 hours |
Elimination half-life |
90 minutes | 7 hours |
17β-HSD ? |
Yes | No |
| Bound to SHBG? | Yes | No |
| Relative oral liver potency | 1 | ~500–1,500 |
| Relative oral pituitary potency | 1 | 200 |
| Sources:[70] | ||
Pharmacokinetics
Absorption

The
EE levels after a single 50 μg dose by intravenous injection are several times higher than levels of EE after a single 50 mg dose given orally.[153] Besides the difference in levels, the course of elimination is similar for the two routes.[153]
There may be gender-specific differences in the
Distribution
The plasma protein binding of EE is 97 to 98%, and it is bound almost exclusively to albumin.[5][7][10][154] Unlike estradiol, which binds with high affinity to SHBG, EE has very low affinity for this protein, about 2% of that of estradiol, and hence does not bind to it importantly.[155]
Metabolism
Due to high first-pass metabolism in the
Aside from sulfate conjugation, EE is mainly
Unlike the case of estradiol, in which there is a rapid rise in its levels and which remain elevated in a plateau-like curve for many hours, levels of EE fall rapidly after peaking.
EE, following
Elimination
EE is
Chemistry
EE, also known as 17α-ethynylestradiol or as 17α-ethynylestra-1,3,5(10)-triene-3,17β-diol, is a
(17α-methyltestosterone).Analogues
A number of
History
EE was the first orally active synthetic estrogen and was described in 1938 by Hans Herloff Inhoffen and Walter Hohlweg of Schering AG in Berlin.[159][160][161][162][163] It was approved by the US Food and Drug Administration (FDA) in June 1943, and marketed by Schering under the brand name Estinyl.[14] The FDA withdrew approval of Estinyl effective 4 June 2004 at the request of Schering, which had discontinued marketing it.[164]
EE was never introduced for use by intramuscular injection.[165]
EE was first used in COCs, as an alternative to mestranol, in 1964, and shortly thereafter superseded mestranol in COCs.[15]
Early COCs contained 40 to 100 μg/day EE and 50 to 150 μg/day mestranol.[166][167]
Society and culture
Generic names
Ethinylestradiol is the
The name of the drug is often abbreviated as EE or as EE2 in the medical literature.
Brand names
EE has been marketed as a standalone oral drug under the brand names Esteed, Estinyl, Feminone, Lynoral, Menolyn, Novestrol, Palonyl, Spanestrin, and Ylestrol among others, although most or all of these formulations are now discontinued.
Availability
Ethinylestradiol is marketed throughout the world.[168][158] It is marketed exclusively or almost exclusively in combination with progestins.[168]
References
- ^ ISBN 978-1-4757-2085-3.
- ^ PMID 2256522.
- ^ PMID 22468839.
- ^ PMID 8842581.
- ^ ISBN 978-1-57439-179-4.
- ISBN 978-1-56363-429-1.
- ^ S2CID 24616324.
- ^ ISBN 978-3-642-60107-1.
The binding affinity of EE2 for the estrogen receptor is similar to that of estradiol. [...] During daily intake, the EE2 levels increase up to a steady state which is reached after about 1 week.
- ^ ISBN 978-3-319-27449-2.
- ^ PMID 23375353.
- ^ ISBN 978-94-010-8339-3.
Ethinyl estradiol is a synthetic and comparatively potent estrogen. As a result of the alkylation in 17-C position it is not a substrate for 17β dehydrogenase, an enzyme which transforms natural estradiol-17β to the less potent estrone in target organs.
- ^ a b c d "Drugs@FDA: FDA Approved Drug Products". U.S. Food and Drug Administration (FDA). Retrieved 22 December 2016.
- ISBN 978-3-527-60749-5.
- ^ a b U.S. Food and Drug Administration (FDA) (2007). "Approval history: Estinyl (ethinyl estradiol) NDA 005292". search: Estinyl
- ^ ISBN 978-1-4899-3496-3.
In 1964, ethinyl estradiol was introduced as an alternative to mestranol as the estrogenic component, [...]
- PMID 25841596.
- ISBN 978-1-4612-2730-4.
- ^ a b c d e f g "The Top 300 of 2021". ClinCalc. Archived from the original on 15 January 2024. Retrieved 14 January 2024.
- ^ "Ethinyl Estradiol; Norethindrone - Drug Usage Statistics". ClinCalc. Retrieved 14 January 2024.
- ^ "Ethinyl Estradiol; Norgestimate - Drug Usage Statistics". ClinCalc. Retrieved 14 January 2024.
- ^ "Ethinyl Estradiol; Levonorgestrel - Drug Usage Statistics". ClinCalc. Retrieved 14 January 2024.
- ^ "Ethinyl Estradiol ; Etonogestrel - Drug Usage Statistics". ClinCalc. Retrieved 14 January 2024.
- ^ "Ethinyl Estradiol ; Norgestrel - Drug Usage Statistics". ClinCalc. Retrieved 14 January 2024.
- ^ "Ethinyl Estradiol; Ethynodiol - Drug Usage Statistics". ClinCalc. Archived from the original on 18 January 2024. Retrieved 14 January 2024.
- ^ "Drospirenone; EthinylEstradiol; Levomefolate - Drug Usage Statistics". ClinCalc. Retrieved 14 January 2024.
- ^ PMID 16860174.
- .
- ^ PMID 28078219.
- ^ PMID 27889048.
- S2CID 14949511.
- S2CID 10971754.
- ^ "Menopausal Hormone Therapy and Cancer Risk". American Cancer Society. 13 February 2015.
- ^ ISBN 978-92-832-1291-1.
- ^ ISBN 978-0-7817-1750-2.
- ISBN 978-0-7881-0405-3.
ETHINYL ESTRADIOL: TABLET; ORAL: ESTINYL: SCHERING: 0.02MG; 0.05MG; 0.5MG
- OCLC 7074861.
- ISBN 978-3-7692-2114-5.
Ethinyl oestradiol 0,05mg cpr 0,05 mg ethinylestradiol (G03CA01) (FR) Ethinylestradiol tablets 50 mcg Ethinylestradiol (G03CA01) (RUS) Ethinylestradiol 25μg (Jenapharm) Dragees: Ethinylestradiol 25μg (G03CA01) (DE) Ethinylestradiol pch 0,002mg cpr 0,002 mg ethinylestradiol (FR) Ethinylestradiolum tablet 0,05mg ethinylestradiol 0,05 mg (G03CA01) (NL) [...] Etifollin tab 0,5mg (Nycomed pharma a/s) ethinylestradiol (L02AA03) (NO) Etifollin tab 50mcg (Nycomed pharma a/s) ethinylestradiol (G03CA01) (NO)
- OCLC 1058058829.
Ethinyloestradiol (Lynoral, 0.05-mg, 0.1-mg, 1-mg tablets)
- ^ ISBN 978-0-323-07067-6.
- ^ ISBN 978-1-60913-713-7.
- ^ "U.S. Selected Practice Recommendations for Contraceptive Use, 2016" (PDF). Recommendations and Reports. Vol. 65, no. 4. Centers for Disease Control and Prevention. 29 July 2016.
- ^ "U.S. Selected Practice Recommendations for Contraceptive Use, 2016" (PDF). Recommendations and Reports. Vol. 65, no. 4. Centers for Disease Control and Prevention. 29 July 2016.
- ^ a b "U.S. Medical Eligibility Criteria for Contraceptive Use, 2016" (PDF). Recommendations and Reports. Vol. 65, no. 3. Centers for Disease Control and Prevention. 29 July 2016.
- ^ ISBN 978-0-08-093292-7.
- ^ PMID 1983896.
- ^ ISBN 978-3-662-07635-4.
- ^ PMID 1983923.
- PMID 23904209.
- ISBN 978-1-4832-7064-7.
- ISBN 978-3-642-60107-1.
- ^ ISBN 978-0-08-092150-1.
- ^ ISBN 978-1-119-03909-9.
- ^ PMID 27793376.
- ^ PMID 23384743.
- PMID 32431379.
- ^ ISBN 978-0-323-03309-1.
- PMID 28376481.
- ISBN 978-0-7817-1750-2.
Low-dose COCs contain <50 μg of estrogen and are the primary choice for oral contraception. COCs containing ≥50 μg of estrogen should no longer be routinely used for contraception. [...] The estrogen component of COCs can cause breast fullness and tenderness.
- ISBN 978-0-309-04493-6. NAP:13774.
Following a recommendation by its Fertility and Maternal Health Drugs Advisory Committee, the Food and Drug Administration (FDA) recently ordered the removal from the market of all oral contraceptives with [ethinylestradiol] contents greater than 50 μg.
- ISBN 978-1-4379-4231-6.
Oral contraceptive formulations containing greater than 50 ug ethinyl estradiol were removed from the United States market in 1989, and currently marketed formulations generally contain between 20 and 35 μg ethinyl estradiol.
- PMID 27678035.
- PMID 23904209.
- ^ PMID 12047300.
- S2CID 20803995.
- PMID 18692609.
- ^ ISBN 978-3-319-53298-1.
- PMID 16915215.
- PMID 22011208.
- ^ S2CID 32650111.
- ^ S2CID 21510744.
- ^ PMID 3817605.
- ^ ]
- ^ PMID 24932461.
- ^ ISBN 978-1-60795-014-1.
- ^ PMID 28667081.
- ISBN 978-0-306-48240-3.
- ^ ISBN 978-0-470-98697-4.
- ^ ISSN 0171-2004.
- ISBN 978-3-527-32363-0.
- ^ S2CID 73398961.
- PMID 30020636.
- ^ S2CID 7932937.
- S2CID 128359413.
- S2CID 260318275.
- ^ ISBN 978-1-4757-1767-9.
- ISBN 978-1-4613-0867-6.
- ^ PMID 17517636.
- ^ S2CID 32669410.
- S2CID 86245855.
- ^ S2CID 71784426.
- PMID 16554039.
- PMID 21321128.
- PMID 26023144.
- PMID 20403194.
- PMID 21844907.
Further research showed that the therapeutic effect of ethynylestradiol in established EAE was mediated via GPER, but not via ERα, and possibly involved production of the anti-inflammatory cytokine Il‑10.115
- PMID 24530924.
In addition, the therapeutic effect of ethinyl estradiol in established disease was demonstrated to require expression of GPER but not ERα, and was associated with the production of the anti-inflammatory cytokine IL-10 (Yates et al., 2010).
- PMID 23841731.
- ISBN 978-0-7817-3762-3.
- ISBN 978-1-904798-74-3.
- ^ ISBN 978-0-683-03631-2.
The synthetic estrogen, ethinyl estradiol, more commonly used in oral contraceptives, has a biological activity 100 times that of the native and conjugated substances.
- ^ ISBN 978-1-59745-150-5.
EE2 has about 100 times the potency of an equivalent weight of conjugated equine estrogen or estrone sulfate for stimulating synthesis of hepatic proteins. [...] EE2 is about 1.7 times as potent as the same weight of mestranol.
- ISBN 978-1-4899-1133-9.
Meyer et al. found that ethinyl estradiol was 75 to 100 times more potent than conjugated estrogen on the basis of the doses required to lower testosterone to the adult female range, 0.1 mg of the former and 7.5 to 10 mg of the latter being necessary.
- ISBN 978-0-397-51418-2.
The relative potency of several estrogens has been assayed by determination of effects on plasma FSH, a measure of the systemic effect, and by increases in SHBG, CBG, and angiotensinogen, all of which indicate the hepatic effect. Piperazine estrone sulfate and micronized estradiol were equipotent with respect to increases in SHBG, whereas conjugated estrogens were 3.2-fold more potent, DES was 28.4-fold more potent, and ethinyl estradiol was 600-fold more potent. With respect to decreased FSH, conjugated estrogens were 1.4-fold, DES was 3.8-fold, and ethinyl estradiol was 80 to 200-fold more potent than was piperazine estrone sulfate.
- ^ PMID 6291391.
- PMID 2215269.
- PMID 559617.
- ISBN 978-3-642-75101-1.
- ISBN 978-3-11-024568-4.
- ISBN 978-3-662-00942-0.
- ISBN 978-94-009-8195-9.
- ISBN 978-3-11-150424-7.
- PMID 779393.
- ISSN 0001-6349.
- ISSN 0172-777X.
- PMID 29603164.
- PMID 29756046.
- PMID 15432047.
- PMID 14902290.
- ISSN 0001-6349.
There is no doubt that the conversion of the endometrium with injections of both synthetic and native estrogenic hormone preparations succeeds, but the opinion whether native, orally administered preparations can produce a proliferation mucosa changes with different authors. PEDERSEN-BJERGAARD (1939) was able to show that 90% of the folliculin taken up in the blood of the vena portae is inactivated in the liver. Neither KAUFMANN (1933, 1935), RAUSCHER (1939, 1942) nor HERRNBERGER (1941) succeeded in bringing a castration endometrium into proliferation using large doses of orally administered preparations of estrone or estradiol. Other results are reported by NEUSTAEDTER (1939), LAUTERWEIN (1940) and FERIN (1941); they succeeded in converting an atrophic castration endometrium into an unambiguous proliferation mucosa with 120–300 oestradiol or with 380 oestrone.
- ISBN 978-3-642-57636-2.
- ^ Martinez-Manautou J, Rudel HW (1966). "Antiovulatory Activity of Several Synthetic and Natural Estrogens". In Robert Benjamin Greenblatt (ed.). Ovulation: Stimulation, Suppression, and Detection. Lippincott. pp. 243–253.
- ISBN 978-3-642-49506-9.
- PMID 13370006.
- ^ PMID 4359746.
- ^ ISSN 2380-548X.
- ^ ISBN 978-1-107-01290-5.
- PMID 22294742.
- PMID 18338653.
- PMID 24082040.
- S2CID 259361637.
- S2CID 44335732.
- ^ PMID 7000222.
- ^ S2CID 33063805.
- S2CID 40497389.
- ^ ISBN 978-1-4557-1126-0.
- ISBN 978-1-85317-422-3.
- S2CID 4492779.
- PMID 4568621.
- ISBN 978-3-642-57636-2.
- PMID 4574573.
- S2CID 53246678.
- ISBN 978-0-397-59010-0.
- ISBN 978-3-642-49506-9.
- PMID 1146927.
- ^ ISBN 978-1-59259-101-5.
- ^ S2CID 6815423.
- PMID 22244780.
- ^ ISBN 978-0-08-055309-2.
- ISBN 978-1-4443-4263-5.
- S2CID 23760705.
- ^ S2CID 27729272.
- ^ ISBN 978-0-19-979361-7.
- ^ S2CID 43298472.
- ^ ISBN 978-94-009-4145-8.
- PMID 7195405.
- S2CID 73487051.
- ^ S2CID 11212469.
- ^ ISBN 978-3-88763-075-1.
- S2CID 46648877.
- OCLC 543168.
- PMID 4098492.
- ISBN 978-0-471-89980-8.
- PMID 16389046.
- ^ U.S. Food and Drug Administration (FDA) (5 May 2004). "Schering Corp. et al.; Withdrawal of Approval of 92 New Drug Applications and 49 Abbreviated New Drug Applications. Notice" (PDF). Federal Register. 69 (87): 25124–30.
- PMID 13359169.
- ISBN 978-0-387-90087-2.
- ISBN 978-3-642-99942-0.
- ^ a b c d e f g "Ethinylestradiol - Drugs.com".
- ISBN 978-94-011-4439-1.
- ISBN 978-0-88416-175-2.
Ethinyl Estradiol [Estinyl, Feminone, Lynoral, Novestrol, Palonyl]
- ISBN 978-0-930530-02-0.
ETHINYL ESTRADIOL U.S.P. (Esteed®, Estinyl®, Lynoral®, Menolyn®, Novestrol®, Palonyl®, Spanestrin®, Ylestrol®)
Further reading
- Oettel M, Schillinger E (6 December 2012). Estrogens and Antiestrogens II: Pharmacology and Clinical Application of Estrogens and Antiestrogen. Springer Science & Business Media. pp. 4, 10, 15, 165, 247–248, 276–291, 363–408, 424, 514, 540, 543, 581. ISBN 978-3-642-60107-1.
- Kuhl H (August 2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration". Climacteric. 8 (Suppl 1): 3–63. S2CID 24616324.
- Stanczyk FZ, Archer DF, Bhavnani BR (June 2013). "Ethinyl estradiol and 17β-estradiol in combined oral contraceptives: pharmacokinetics, pharmacodynamics and risk assessment". Contraception. 87 (6): 706–727. PMID 23375353.
- Mattison DR, Karyakina N, Goodman M, LaKind JS (September 2014). "Pharmaco- and toxicokinetics of selected exogenous and endogenous estrogens: a review of the data and identification of knowledge gaps". Critical Reviews in Toxicology. 44 (8): 696–724. S2CID 11212469.
