CYP3A4
Ensembl |
| ||||||||
|---|---|---|---|---|---|---|---|---|---|
| UniProt |
| ||||||||
| RefSeq (mRNA) |
| ||||||||
| RefSeq (protein) |
| ||||||||
| Location (UCSC) | Chr 7: 99.76 – 99.78 Mb | n/a | |||||||
| PubMed search | [2] | n/a | |||||||
| View/Edit Human | |||
Cytochrome P450 3A4 (abbreviated CYP3A4) (EC 1.14.13.97) is an important enzyme in the body, mainly found in the liver and in the intestine, which in humans is encoded by CYP3A4 gene. It oxidizes small foreign organic molecules (xenobiotics), such as toxins or drugs, so that they can be removed from the body. It is highly homologous to CYP3A5, another important CYP3A enzyme.
While many drugs are deactivated by CYP3A4, there are also some drugs that are activated by the enzyme. Some substances, such as some drugs and furanocoumarins present in grapefruit juice, interfere with the action of CYP3A4. These substances will, therefore, either amplify or weaken the action of those drugs that are modified by CYP3A4.
CYP3A4 is a member of the
Function
CYP3A4 is a member of the
The CYP3A4 protein localizes to the
CYP3A4 also possesses
Evolution
The CYP3A4 gene exhibits a much more complicated upstream regulatory region in comparison with its
Tissue distribution
Fetuses do not express CYP3A4 in their liver tissue, but rather CYP3A7 (EC 1.14.14.1), which acts on a similar range of substrates. CYP3A4 increases to approximately 40% of adult levels in the fourth month of life and 72% at 12 months.[13][14]
Although CYP3A4 is predominantly found in the liver, it is also present in other organs and tissues of the body, where it may play an important role in metabolism. CYP3A4 in the intestine plays an important role in the metabolism of certain drugs. Often this allows
Recently CYP3A4 has also been identified in the brain, but its role in the central nervous system is still unknown.[15]
Mechanisms
Cytochrome P450 enzymes perform an assortment of modifications on a variety of ligands, utilizing its large active site and its ability to bind more than one substrate at a time to perform complicated chemical alterations in the metabolism of endogenous and exogenous compounds. These include hydroxylation, epoxidation of olefins, aromatic oxidation, heteroatom oxidations, N- and O- dealkylation reactions, aldehyde oxidations, dehydrogenation reactions, and aromatase activity.[16][17]
Hydroxylation of an
Two mechanisms have been proposed as the primary pathway of hydroxylation in P450 enzymes.
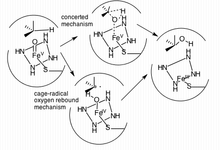
The first pathway suggested is a cage-controlled radical method ("oxygen rebound"), and the second involves a concerted mechanism that does not utilize a radical intermediate but instead acts very quickly via a "radical clock".[18]
Inhibition through fruit ingestion
In 1998, various researchers showed that grapefruit juice, and grapefruit in general, is a potent inhibitor of CYP3A4, which can affect the metabolism of a variety of drugs, increasing their bioavailability.[19][20][21][22][23] In some cases, this can lead to a fatal interaction with drugs like astemizole or terfenadine.[20] The effect of grapefruit juice with regard to drug absorption was originally discovered in 1989. The first published report on grapefruit drug interactions was in 1991 in the Lancet entitled "Interactions of Citrus Juices with Felodipine and Nifedipine", and was the first reported food-drug interaction clinically. The effects of grapefruit last from 3–7 days, with the greatest effects when juice is taken an hour previous to administration of the drug.[24]
In addition to grapefruit, other fruits have similar effects.
Variability
While over 28
CYP3A4 alleles that have been reported to have minimal function compared to wild-type include CYP3A4*6 (an A17776 insertion) and CYP3A4*17 (F189S). Both of these SNPs led to decreased catalytic activity with certain ligands, including testosterone and nifedipine in comparison to wild-type metabolism.[28] By contrast, CYP3A4*1G allele has more potent enzymatic activity compared to CYP3A4*1A (the wild-type allele).[29]
Variability in CYP3A4 function can be determined noninvasively by the erythromycin breath test (ERMBT). The ERMBT estimates in vivo CYP3A4 activity by measuring the radiolabelled carbon dioxide exhaled after an intravenous dose of (14C-N-methyl)-erythromycin.[30]
Induction
CYP3A4 is
Induction of CYP3A4 has been shown to vary in humans depending on sex. Evidence shows an increased drug clearance by CYP3A4 in women, even when accounting for differences in body weight. A study by Wolbold et al. (2003) found that the median CYP3A4 levels measured from surgically removed liver samples of a random sample of women exceeded CYP3A4 levels in the livers of men by 129%. CYP3A4 mRNA transcripts were found in similar proportions, suggesting a pre-translational mechanism for the up-regulation of CYP3A4 in women. The exact cause of this elevated level of enzyme in women is still under speculation, however studies have elucidated other mechanisms (such as CYP3A5 or CYP3A7 compensation for lowered levels of CYP3A4) that affect drug clearance in both men and women.[32]
CYP3A4 substrate activation varies amongst different animal species. Certain ligands activate human PXR, which promotes CYP3A4 transcription, while showing no activation in other species. For instance, mouse PXR is not activated by rifampicin and human PXR is not activated by pregnenolone 16α-carbonitrile[33] In order to facilitate study of CYP3A4 functional pathways in vivo, mouse strains have been developed using transgenes in order to produce null/human CYP3A4 and PXR crosses. Although humanized hCYP3A4 mice successfully expressed the enzyme in their intestinal tract, low levels of hCYP3A4 were found in the liver.[33] This effect has been attributed to CYP3A4 regulation by the growth hormone signal transduction pathway.[33] In addition to providing an in vivo model, humanized CYP3A4 mice (hCYP3A4) have been used to further emphasize gender differences in CYP3A4 activity.[33]
CYP3A4 activity levels have also been linked to diet and environmental factors, such as duration of exposure to xenobiotic substances.[34] Due to the enzyme's extensive presence in the intestinal mucosa, the enzyme has shown sensitivity to starvation symptoms and is upregulated in defense of adverse effects. Indeed, in fatheaded minnows, unfed female fish were shown to have increased PXR and CYP3A4 expression, and displayed a more pronounced response to xenobiotic factors after exposure after several days of starvation.[34] By studying animal models and keeping in mind the innate differences in CYP3A4 activation, investigators can better predict drug metabolism and side effects in human CYP3A4 pathways.
Turnover
Estimates of the turnover rate of human CYP3A4 vary widely. For hepatic CYP3A4, in vivo methods yield estimates of the enzyme half-life mainly in the range of 70 to 140 hours, whereas in vitro methods give estimates from 26 to 79 hours.[35] Turnover of gut CYP3A4 is likely to be a function of the rate of enterocyte renewal; an indirect approach based on the recovery of activity following exposure to grapefruit juice yields measurements in the 12- to 33-hour range.[35]
Technology
Due to membrane-bound CYP3A4's natural propensity to conglomerate, it has historically been difficult to study drug binding in both solution and on surfaces. Co-crystallization is difficult since the substrates tend to have a low KD (between 5–150 μM) and low solubility in aqueous solutions.[36] A successful strategy in isolating the bound enzyme is the functional stabilization of monomeric CYP3A4 on silver nanoparticles produced from nanosphere lithography and analyzed via localized surface plasmon resonance spectroscopy (LSPR).[37] These analyses can be used as a high-sensitivity assay of drug binding, and may become integral in further high-throughput assays utilized in initial drug discovery testing. In addition to LSPR, CYP3A4-Nanodisc complexes have been found helpful in other applications including solid-state NMR, redox potentiometry, and steady-state enzyme kinetics.[37]
Ligands
Following are lists of selected
Substrates
The substrates of CYP3A4 are:
- some immunosuppressants:
- ciclosporin (cyclosporin),[38][39]
- tacrolimus,[38][39]
- sirolimus,[38][39]
- upadacitinib;[40][41]
- many chemotherapeutics:
- docetaxel,[38][39]
- tamoxifen,[38][39]
- paclitaxel,[38][39]
- cyclophosphamide,[39]
- doxorubicin,[39]
- erlotinib,[42]
- etoposide,[39]
- ifosfamide,[39]
- teniposide,[39]
- vinblastine,[39]
- vincristine,[38]
- vindesine,[39]
- imatinib,[38]
- irinotecan,[38]
- sorafenib,[38]
- sunitinib,[38]
- vemurafenib,[38]
- temsirolimus,[38]
- anastrozole,
- gefitinib;
- azole antifungals:
- macrolides (except azithromycin):[38]
- dapsone[38] (in leprosy),
- tricyclic antidepressants:
- SSRI antidepressants :
- citalopram[39]
- norfluoxetine[39]
- sertraline[39]
- some other antidepressants:
- mirtazapine[39] (NaSSA),
- nefazodone[39] (atypical),
- reboxetine[39] (NRI),
- SNRI),
- trazodone[38] (SARI),
- vilazodone[39] (serotonin modulator),
- buspirone[38][39] (anxiolytic),
- antipsychotics:
- opioids(mainly analgesics):
- alfentanil,[38][39]
- buprenorphine[45] (analgesic, addiction maintenance treatment),
- antitussive, antidiarrheal),
- fentanyl,[38]
- hydrocodone[46] (partial involvement, not the bioactivation factor),
- methadone[38] (analgesic, addiction maintenance treatment),
- levacetylmethadol,[38]
- tramadol (to inactive metabolites, do not confuse with metabolism via CYP2D6);
- benzodiazepines:
- some hypnotics:
- donepezil[39] (acetylcholinesterase inhibitor),
- statins (except pravastatin[38] and rosuvastatin[38]):
- calcium channel blockers:
- sensitive substrate[48]),
- felodipine[38][39] (sensitive substrate[49][50][51][52]),
- nifedipine[38][39] (sensitive substrate[53][54][55][56]),
- verapamil[38][39] (sensitive substrate[57][58][59][60][61][62][63]),
- amlodipine[38] (sensitive substrate[64]),
- lercanidipine,[38]
- nitrendipine,[38]
- nisoldipine,[38]
- class III antiarrhythmic),
- class III antiarrhythmic),
- class I antiarrhythmic),
- PDE5 inhibitors:
- vasodilators, smooth musclecontractors),
- steroids:
- sex hormones(agonists and antagonists):
- finasteride[38][39] (antiandrogen),
- estradiol[38] (estrogen),
- progesterone,[38]
- hormonal contraceptive),
- testosterone[38] (androgen),
- toremifene[39] (SERM),
- bicalutamide;[66]
- glucocorticoids:
- some H1-receptor antagonists (H1 antihistamines):
- protease inhibitors:
- non-nucleoside antiretroviral drugs):
- antihelminthic)
- cisapride,[38][39] (5-HT4 receptor agonist)
- aprepitant,[38] (antiemetic)
- caffeine,[38] (stimulant)
- cocaine,[38] (stimulant)
- cilostazol,[38] (phosphodiesterase inhibitor)
- antitussive)
- antidopaminergic)
- aldosterone antagonist)
- antiarrhythmic)
- ondansetron,[38] (5-HT3 antagonist)
- propranolol,[38] (beta blocker)
- beta agonist)
- warfarin,[73] (anticoagulant)
- antiplatelet),
- 2-oxo-clopidogrel,[29]
- proton pump inhibitor)
- antidiabetic)
- methoxetamine,[75]
- leukotriene receptor antagonist),
- vilaprisan (selective progesterone receptor modulator),
- certain angiotensin II receptor blockers:
Inhibitors
Inhibitors of CYP3A4 are classified by potency:
- a Strong inhibitor causes at least a 5-fold increase in the plasma clearance.[38]
- a Moderate inhibitor causes at least a 2-fold increase in the plasma AUC values, or 50–80% decrease in clearance.[38]
- a Weak inhibitor causes at least a 1.25-fold but less than 2-fold increase in the plasma AUC values, or 20–50% decrease in clearance.[38]
The inhibitors of CYP3A4 are the following substances.
Strong inhibitors
- boceprevir,[78]
- protease inhibitors:
- some macrolide antibiotics:[79]
- clarithromycin,[78][80][81][38][39][82][83]
- erythromycin[83] (although FDA lists it as a moderate inhibitor, and inhibitor of P-glycoprotein, defined as those increasing the AUC of digoxin to ≥1.25-fold);[78]
- telithromycin
- ceritinib
- angina pectoris)
- nefazodone (antidepressant)
- ribociclib
- tucatinib
- chloramphenicol (antibiotic)[84]
- some azole antifungals:
- cobicistat,[85]
- green tea extract,[86][87][88]
- grape seed extract,[86][87][88]
- dillapiole (compound present in dill plants),[89][90]
- apigenin (compound present in plants such as celery, parsley, and chamomile)[91]
- Artemisia annua[92]
Moderate inhibitors
- class III antiarrhythmic),[85]
- aprepitant,[78] (antiemetic)
- ciprofloxacin,[78]
- conivaptan,[78]
- crizotinib,[78]
- rutin (in vitro)[93][94] (dietary flavonoid),
- tofisopam,[78]
- some calcium channel blockers:
- some azole antifungals:[79]
- bergamottin[96][38] (constituent of grapefruit juice),
- cyclosporine,[85]
- donedarone,[85]
- fluvoxamine,[85]
- imatinib,[85]
- valerian.[97]
Weak inhibitors
- berberine[98][99][100][101] (an alkaloid found in plants such as berberis or goldenseal),
- buprenorphine (analgesic),[102]
- cafestol (in unfiltered coffee)[103]
- cilostazol,[85]
- cimetidine,[85]
- fosaprepitant,[85]
- lomitapide,[85]
- orphenadrine,
- proton pump inhibitor),
- quercetin,[104][38]
- ranitidine,[85]
- ranolazine,[85]
- tacrolimus,[85]
- ticagrelor,[85]
- valproic acid,[105]
- amlodipine,[64]
- macrolide antibiotic).[83]
Inhibitors of unspecified potency
- cannabidiol,[107]
- dithiocarbamate[38] (functional group),
- flavonoids,[108]
- mifepristone[38] (abortifacient),
- norfloxacin[38] (fluoroquinolone antibiotic),
- some non-nucleoside reverse-transcriptase inhibitors:[109]
- hormonal contraceptive),
- star fruit,[38][110]
- milk thistle,[111]
- niacinamide (nicotinamide), collectively called as Vitamin B3,
- ginkgo biloba,[113]
- sesamin[114] (a lignan constituent in sesame seeds and oil),
- piperine,[115]
- isoniazid,[116]
- serenoa.[117]
Inducers
Strong and moderate CYP3A4 inducers are drugs that decrease the AUC of sensitive substrates of a given pathway where CYP3A4 is involved by ≥80 percent and ≥50 to <80 percent, respectively.[78][118] Weak inducers decrease the AUC by ≥20 to <50 percent.[118]
The inducers of CYP3A4 are the following substances.
Strong inducers
- carbamazepine,[78][79]
- antiandrogens:
- phenytoin[78][120] (anticonvulsant),
- rifampin.[78]
Weak inducers
Inducers of unspecified potency
- mood stabilizers:
- barbiturates:[79]
- some bactericidals:
- some non-nucleoside reverse-transcriptase inhibitors:[109]
- hypoglycemic),
- immunosuppressive),
- modafinil[67][38] (stimulant),
- capsaicin,[122]
- brigatinib,[38]
- clobazam,[38]
- dabrafenib,[38]
- elagolix,[38]
- eslicarbazepine,[38]
- letermovir,[38]
- lorlatinib,[38]
- oritavancin,[38]
- perampanel,[38]
- telotristat.[38]
Interactive pathway map
Click on genes, proteins and metabolites below to link to respective articles. [§ 1]
- ^ The interactive pathway map can be edited at WikiPathways: "IrinotecanPathway_WP229".
See also
- List of drugs affected by grapefruit
References
- ^ a b c GRCh38: Ensembl release 89: ENSG00000160868 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- PMID 8269949.
- PMID 1391968.
- ^ a b c d
 This article incorporates public domain material from "CYP3A4 cytochrome P450 family 3 subfamily A member 4 [ Homo sapiens (human) ]". Reference Sequence collection. National Center for Biotechnology Information.
This article incorporates public domain material from "CYP3A4 cytochrome P450 family 3 subfamily A member 4 [ Homo sapiens (human) ]". Reference Sequence collection. National Center for Biotechnology Information.
- PMID 23333322.
- ^ EntrezGene 1576
- (PDF) from the original on 18 January 2024. Retrieved 2 February 2024.
- PMID 25244930.
- PMID 11375247.
- ^ S2CID 205602787.
- ^ PMID 19299527.
- S2CID 25596506.
- S2CID 9714442.
- S2CID 17209434.
- PMID 9351897.
- ^ PMID 22677141.
- ^ S2CID 33927145.
- PMID 9548795.
- ^ PMID 9723817.
- S2CID 27490726.
- S2CID 11525439.
- PMID 17112309.
- S2CID 29029956.
- ^ "Integrative Medicine, Noni". Memorial Sloan-Kettering Cancer Center. Archived from the original on 20 August 2013. Retrieved 27 June 2013.
- S2CID 7997718.
- PMID 31924158.
- from the original on 29 July 2020. Retrieved 25 May 2020.
- ^ a b Alkattan A, Alsalameen E. Polymorphisms of genes related to phase-I metabolic enzymes affecting the clinical efficacy and safety of clopidogrel treatment. Expert Opin Drug Metab Toxicol. 2021 Apr 30. doi: 10.1080/17425255.2021.1925249. Epub ahead of print. PMID 33931001.
- PMID 7987401.
- PMID 21641981.
- PMID 14512885.
- ^ from the original on 29 July 2020. Retrieved 6 September 2019.
- ^ PMID 21664292.
- ^ PMID 18537575.
- PMID 22157006.
- ^ PMID 19364136.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc bd be bf bg bh bi bj bk bl bm bn bo bp bq br bs bt bu bv bw bx by bz ca cb cc cd ce cf cg ch ci cj ck cl cm cn co cp cq cr cs ct cu cv cw cx cy cz da db dc dd de df dg dh di dj dk dl dm dn Flockhart DA (2007). "Drug Interactions: Cytochrome P450 Drug Interaction Table". Indiana University School of Medicine. Archived from the original on 10 October 2007. Retrieved 25 December 2008. Retrieved on 25 December 2008.
- ^ FASS (drug formulary): Swedish environmental classification of pharmaceuticals Archived 11 June 2002 at the Wayback MachineFacts for prescribers (Fakta för förskrivare). Retrieved July 2011
- ^ a b "Rinvoq: EPAR – Public assessment report Archived 21 July 2020 at the Wayback Machine" (PDF). European Medicines Agency. 5 March 2020. Archived (PDF) from the original on 21 July 2020. Retrieved 21 July 2020.
- ^ a b Austria-Codex (in German). Vienna: Österreichischer Apothekerverlag. 2020. Rinvoq 15 mg Retardtabletten.
- ^ "Erlotinib". Archived from the original on 24 December 2019. Retrieved 10 April 2018.
Metabolized primarily by CYP3A4 and, to a lesser degree, by CYP1A2 and the extrahepatic isoform CYP1A1
- ^ "Cyclobenzaprine". DrugBank. Archived from the original on 27 October 2018. Retrieved 10 April 2018.
- from the original on 18 May 2023. Retrieved 14 October 2022.
- PMID 19773542.
- PMID 14998425.
- S2CID 22229823.
- PMID 9223567.
- ^ "Drug Development and Drug Interactions: Table of Substrates, Inhibitors and Inducers". U S Food and Drug Administration Home Page. 25 June 2009. Archived from the original on 23 April 2019. Retrieved 1 February 2019.
- PMID 9153299.
- S2CID 1246705.
- PMID 2061924.
- PMID 11231118.
- S2CID 6823063.
- S2CID 30463290.
- ^ "NIFEDIPINE EXTENDED RELEASE- nifedipine tablet, extended release". DailyMed. 29 November 2012. Archived from the original on 31 January 2022. Retrieved 1 February 2019.
Drug Interactions: Nifedipine is mainly eliminated by metabolism and is a substrate of CYP3A. Inhibitors and inducers of CYP3A can impact the exposure to nifedipine and, consequently, its desirable and undesirable effects. In vitro and in vivo data indicate that nifedipine can inhibit the metabolism of drugs that are substrates of CYP3A, thereby increasing the exposure to other drugs. Nifedipine is a vasodilator, and coadministration of other drugs affecting blood pressure may result in pharmacodynamic interactions.
- PMID 9531525.
- S2CID 8942097.
- PMID 2315261.
- S2CID 20446675.
- S2CID 39570845.
- PMID 3358901.
- PMID 3252045.
- ^ S2CID 24304693.
- ^ "Active ingredient: Tadalafil - Brands, Medical Use, Clinical Data". Druglib.com. Archived from the original on 28 November 2022. Retrieved 13 March 2022.
- S2CID 29912565.
- ^ PMID 34633961.
- PMID 31427846.
- PMID 11259984.
- ^ ISBN 978-0-12-802025-8. Retrieved 6 February 2024.
- ^ Enzyme 1.14.13.32 Archived 27 March 2017 at the Wayback Machine at KEGG
- ^ "Showing Protein Cytochrome P450 3A4 (HMDBP01018)". Human Metabolome Database. Retrieved 5 August 2017.
- PMID 12724615.
- PMID 12515739.
- S2CID 27966043.
- ^ "LOSARTAN- losartan potassium tablet, film coated". DailyMed. 26 December 2018. Archived from the original on 7 February 2019. Retrieved 6 February 2019.
- ^ S2CID 26865251.
- ^ a b c d e f g h i j k l m n "Drug Development and Drug Interactions: Table of Substrates, Inhibitors and Inducers". FDA. US Food and Drug Administration. 6 May 2023. Archived from the original on 4 November 2020. Retrieved 21 June 2020.
- ^ ISBN 978-0-443-06911-6.[page needed]
- S2CID 237373341.
- PMID 12152002.
- S2CID 264438050.
- ^ (PDF) from the original on 2 February 2024. Retrieved 2 February 2024.
Erythromycin 500 mg three-four times daily for 6-7 days markedly increased lovastatin exposure (≈6-fold increase in AUC)
- PMID 14576103.
- ^ a b c d e f g h i j k l m n o p q Center for Drug Evaluation and Research. "Drug Interactions & Labeling - Drug Development and Drug Interactions: Table of Substrates, Inhibitors and Inducers". www.fda.gov. Archived from the original on 23 April 2019. Retrieved 6 August 2018.
- ^ PMID 33198812.
- ^ PMID 15499196.
- ^ from the original on 21 October 2023. Retrieved 14 October 2023.
- PMID 31460189.
- PMID 30558213.
- PMID 34069400.
- PMID 36672740.
- from the original on 18 June 2022. Retrieved 2 February 2024.
- PMID 28539725.
- ^ Product Information: ORAVIG(R) buccal tablets, miconazole buccal tablets. Praelia Pharmaceuticals, Inc (per FDA), Cary, NC, 2013.
- PMID 34570813.
- ^ "Valerian: Health Benefits, Side Effects, Uses, Dose & Precautions". Archived from the original on 16 January 2018. Retrieved 10 April 2018.
- S2CID 235960940.
- PMID 37541764.
- PMID 22855269.
- S2CID 206489481.
- S2CID 16229370.
- ^ Nabekura T, Yamaki T, Kitagawa S (2009). "Interaction of coffee diterpenes, cafestol and kahweol, with human P-glycoprotein" (PDF). AAPS Journal. The American Association of Pharmaceutical Scientists. Archived from the original (PDF) on 21 July 2011.
- S2CID 238257296.
- PMID 11736863.
- PMID 38338457.
- PMID 21356216.
- PMID 38540257.
- ^ a b Non-nucleoside reverse-transcriptase inhibitors have been shown to both induce and inhibit CYP3A4.
- S2CID 17392051.
- ^ "HCVadvocate.org". Archived from the original on 5 March 2010.
- PMID 15081432.
- PMID 19883715.
Ginko Biloba has been shown to contain the potent inhibitor amentoflavone
- PMID 22645625.
- S2CID 7398172.
- S2CID 19299097.
- PMID 27713311.
- ^ PMID 34526892.
- ^ Astellas Pharma US, Inc. (August 2012). "Highlights of Prescribing Information: XTANDI (enzalutamide) capsules for oral use" (PDF). U.S. Food and Drug Administration. Archived (PDF) from the original on 31 July 2018. Retrieved 10 April 2018.
- PMID 21358975.
- S2CID 6915760.
- S2CID 26584141.
External links
- PharmGKB: Annotated PGx Gene Information for CYP3A4
- CYP3A4 substrate prediction
- Human CYP3A4 genome location and CYP3A4 gene details page in the UCSC Genome Browser.
- Overview of all the structural information available in the PDB for UniProt: P08684 (Cytochrome P450 3A4) at the PDBe-KB.
This article incorporates text from the United States National Library of Medicine, which is in the public domain.






