Acne
| Acne | |
|---|---|
| Other names | Acne vulgaris |
retinoids, isotretinoin[8] | |
| Frequency | 633 million affected (2015)[9] |
Acne, also known as acne vulgaris, is a long-term
Susceptibility to acne is primarily genetic in 80% of cases.
Treatments for acne are available, including lifestyle changes, medications, and medical procedures. Eating fewer
In 2015, acne affected approximately 633 million people globally, making it the eighth-most common disease worldwide.[9][18] Acne commonly occurs in adolescence and affects an estimated 80–90% of teenagers in the Western world.[19][20][21] Some rural societies report lower rates of acne than industrialized ones.[21][22] Children and adults may also be affected before and after puberty.[23] Although acne becomes less common in adulthood, it persists in nearly half of affected people into their twenties and thirties, and a smaller group continues to have difficulties in their forties.[2]
Classification
The severity of acne vulgaris (Gr. ἀκμή, "point" + L. vulgaris, "common")
Large nodules were previously called cysts. The term nodulocystic has been used in the medical literature to describe severe cases of inflammatory acne.[25] True cysts are rare in those with acne, and the term severe nodular acne is now the preferred terminology.[25]
Acne inversa (L. invertō, "upside-down") and acne rosacea (rosa, "rose-colored" + -āceus, "forming") are not forms of acne and are alternate names that respectively refer to the skin conditions hidradenitis suppurativa (HS) and rosacea.[26][27][28] Although HS shares certain overlapping features with acne vulgaris, such as a tendency to clog skin follicles with skin cell debris, the condition otherwise lacks the hallmark features of acne and is therefore considered a distinct skin disorder.[26]
Signs and symptoms
Typical features of acne include
Scars
Acne scars are caused by inflammation within the dermis and are estimated to affect 95% of people with acne vulgaris.[31] Abnormal healing and dermal inflammation create the scar.[32] Scarring is most likely to take place with severe acne but may occur with any form of acne vulgaris.[31] Acne scars are classified based on whether the abnormal healing response following dermal inflammation leads to excess collagen deposition or loss at the site of the acne lesion.[33]
Atrophic acne scars have lost collagen from the healing response and are the most common type of acne scar (accounting for approximately 75% of all acne scars).
Hypertrophic scars are uncommon and are characterized by increased collagen content after the abnormal healing response.[32] They are described as firm and raised from the skin.[32][34] Hypertrophic scars remain within the original margins of the wound, whereas keloid scars can form scar tissue outside of these borders.[32] Keloid scars from acne occur more often in men and people with darker skin, and usually occur on the trunk of the body.[32]
In November 2021 a study[35] was published exposing the consensus of twenty-four renowned international plastic surgeons and dermatologists about the most effective energy-based devices for the treatment of acne scars.[36]
Pigmentation
After an inflamed nodular acne lesion resolves, it is common for
Causes
Risk factors for the development of acne, other than genetics, have not been conclusively identified. Possible secondary contributors include hormones, infections, diet, and stress. Studies investigating the impact of smoking on the incidence and severity of acne have been inconclusive.[2][41][42] Sunlight and cleanliness are not associated with acne.[14]
Genes
Acne appears to be highly
Hormones
Hormonal activity, such as occurs during menstrual cycles and puberty, may contribute to the formation of acne. During puberty, an increase in sex hormones called androgens causes the skin follicle glands to grow larger and make more oily sebum.[12] The androgen hormones testosterone, dihydrotestosterone (DHT), and dehydroepiandrosterone (DHEA) are all linked to acne. High levels of growth hormone (GH) and insulin-like growth factor 1 (IGF-1) are also associated with worsened acne.[45] Both androgens and IGF-1 seem to be essential for acne to occur, as acne does not develop in individuals with complete androgen insensitivity syndrome (CAIS) or Laron syndrome (insensitivity to GH, resulting in very low IGF-1 levels).[46][47]
Medical conditions that commonly cause a high-androgen state, such as
Infections
The anaerobic bacterial species Cutibacterium acnes (formerly Propionibacterium acnes) contributes to the development of acne, but its exact role is not well understood.[2] There are specific sub-strains of C. acnes associated with normal skin and others with moderate or severe inflammatory acne.[53] It is unclear whether these undesirable strains evolve on-site or are acquired, or possibly both depending on the person. These strains have the capability of changing, perpetuating, or adapting to the abnormal cycle of inflammation, oil production, and inadequate sloughing of dead skin cells from acne pores. Infection with the parasitic mite Demodex is associated with the development of acne.[30][54] It is unclear whether eradication of the mite improves acne.[54]
Diet
High-
Stress
There are few high-quality studies to demonstrate that stress causes or worsens acne.[61] Despite being controversial, some research indicates that increased acne severity is associated with high stress levels in certain contexts, such as hormonal changes seen in premenstrual syndrome.[62][63]
Other
Some individuals experience severe intensification of their acne when they are exposed to hot humid climates; this is due to bacteria and fungus thriving in warm, moist environments. This climate-induced acne exacerbation has been termed tropical acne. Mechanical obstruction of
Pathophysiology


Acne vulgaris is a chronic skin disease of the
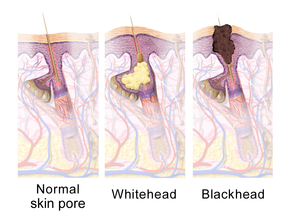
The earliest pathologic change is the formation of a plug (a
The main hormonal driver of oily sebum production in the skin is
C. acnes' ability to bind and activate a class of
C. acnes also provokes skin inflammation by altering the fatty composition of oily sebum.
This inflammatory cascade typically leads to the formation of inflammatory acne lesions, including
Along with the bacteria C. acnes, the bacterial species Staphylococcus epidermidis (S. epidermidis) also takes a part in the physiopathology of acne vulgaris. The proliferation of S. epidermidis with C. acnes causes the formation of
Diagnosis
Acne vulgaris is diagnosed based on a medical professional's clinical judgment.[15] The evaluation of a person with suspected acne should include taking a detailed medical history about a family history of acne, a review of medications taken, signs or symptoms of excessive production of androgen hormones, cortisol, and growth hormone.[15] Comedones (blackheads and whiteheads) must be present to diagnose acne. In their absence, an appearance similar to that of acne would suggest a different skin disorder.[28] Microcomedones (the precursor to blackheads and whiteheads) are not visible to the naked eye when inspecting the skin and require a microscope to be seen.[28] Many features may indicate that a person's acne vulgaris is sensitive to hormonal influences. Historical and physical clues that may suggest hormone-sensitive acne include onset between ages 20 and 30; worsening the week before a woman's period; acne lesions predominantly over the jawline and chin; and inflammatory/nodular acne lesions.[1]
Several scales exist to grade the severity of acne vulgaris, but disagreement persists about the ideal one for diagnostic use.[71][72] Cook's acne grading scale uses photographs to grade severity from 0 to 8, with higher numbers representing more severe acne. This scale was the first to use a standardized photographic protocol to assess acne severity; since its creation in 1979, the scale has undergone several revisions.[72] The Leeds acne grading technique counts acne lesions on the face, back, and chest and categorizes them as inflammatory or non-inflammatory. Leeds scores range from 0 (least severe) to 10 (most severe) though modified scales have a maximum score of 12.[72][73] The Pillsbury acne grading scale classifies the severity of the acne from grade 1 (least severe) to grade 4 (most severe).[71][74]
Differential diagnosis
Many skin conditions can mimic acne vulgaris, and these are collectively known as
Management
Many different treatments exist for acne. These include
Recommended therapies for first-line use in acne vulgaris treatment include topical retinoids, benzoyl peroxide, and topical or oral antibiotics.
People often view acne as a short-term condition, some expecting it to disappear after puberty. This misconception can lead to depending on self-management or problems with long-term adherence to treatment. Communicating the long-term nature of the condition and better access to reliable information about acne can help people know what to expect from treatments.[82][83]
Skin care
In general, it is recommended that people with acne do not wash affected skin more than twice daily.[15] The application of a fragrance-free moisturizer to sensitive and acne-prone skin may reduce irritation. Skin irritation from acne medications typically peaks at two weeks after onset of use and tends to improve with continued use.[15] Dermatologists recommend using cosmetic products that specifically say non-comedogenic, oil-free, and will not clog pores.[15]
Acne vulgaris patients, even those with oily skin,[84] should moisturize in order to support the skin's moisture barrier since skin barrier dysfunction may contribute to acne.[84] Moisturizers, especially ceramide-containing moisturizers, as an adjunct therapy are particularly helpful for the dry skin and irritation that commonly results from topical acne treatment. Studies show that ceramide-containing moisturizers are important for optimal skin care; they enhance acne therapy adherence and complement existing acne therapies.[84] In a study where acne patients used 1.2% clindamycin phosphate / 2.5% benzoyl peroxide gel in the morning and applied a micronized 0.05% tretinoin gel in the evening the overwhelming majority of patients experienced no cutaneous adverse events throughout the study. It was concluded that using ceramide cleanser and ceramide moisturizing cream caused the favorable tolerability, did not interfere with the treatment efficacy, and improved adherence to the regimen.[85] The importance of preserving the acidic mantle and its barrier functions is widely accepted in the scientific community. Thus, maintaining a pH in the range 4.5 - 5.5 is essential in order to keep the skin surface in its optimal, healthy conditions.[86][87][88][89][90]
Diet
Medications
Benzoyl peroxide
Side effects include increased skin photosensitivity, dryness, redness, and occasional peeling.[95] Sunscreen use is often advised during treatment, to prevent sunburn. Lower concentrations of benzoyl peroxide are just as effective as higher concentrations in treating acne but are associated with fewer side effects.[93][96] Unlike antibiotics, benzoyl peroxide does not appear to generate bacterial antibiotic resistance.[95]
Retinoids
Topical retinoids include
Isotretinoin is an oral retinoid that is very effective for severe nodular acne, and moderate acne that is stubborn to other treatments.[1][20] One to two months of use is typically adequate to see improvement. Acne often resolves completely or is much milder after a 4–6 month course of oral isotretinoin.[1] After a single round of treatment, about 80% of people report an improvement, with more than 50% reporting complete remission.[20] About 20% of people require a second course, but 80% of those report improvement, resulting in a cumulative 96% efficacy rate.[20]
There are concerns that isotretinoin is linked to adverse effects, like
Medical authorities strictly regulate isotretinoin use in women of childbearing age due to its known
Antibiotics
People may apply antibiotics to the skin or take them orally to treat acne. They work by killing C. acnes and reducing inflammation.[20][95][105] Although multiple guidelines call for healthcare providers to reduce the rates of prescribed oral antibiotics, many providers do not follow this guidance.[106] Oral antibiotics remain the most commonly prescribed systemic therapy for acne.[106] Widespread broad-spectrum antibiotic overuse for acne has led to higher rates of antibiotic-resistant C. acnes strains worldwide, especially to the commonly used tetracycline (e.g., doxycycline) and macrolide antibiotics (e.g., topical erythromycin).[16][95][105][106] Therefore, dermatologists prefer antibiotics as part of combination therapy and not for use alone.[15]
Commonly used antibiotics, either applied to the skin or taken orally, include clindamycin, erythromycin, metronidazole, sulfacetamide, and tetracyclines (e.g., doxycycline or minocycline).[50] Doxycycline 40 milligrams daily (low-dose) appears to have similar efficacy to 100 milligrams daily and has fewer gastrointestinal side effects.[15] However, low-dose doxycycline is not FDA-approved for the treatment of acne.[107] Antibiotics applied to the skin are typically used for mild to moderately severe acne.[20] Oral antibiotics are generally more effective than topical antibiotics and produce faster resolution of inflammatory acne lesions than topical applications.[1] The Global Alliance to Improve Outcomes in Acne recommends that topical and oral antibiotics are not used together.[105]
Oral antibiotics are recommended for no longer than three months as antibiotic courses exceeding this duration are associated with the development of antibiotic resistance and show no clear benefit over shorter durations.[105] If long-term oral antibiotics beyond three months are used, then it is recommended that benzoyl peroxide or a retinoid be used at the same time to limit the risk of C. acnes developing antibiotic resistance.[105]
The antibiotic dapsone is effective against inflammatory acne when applied to the skin. It is generally not a first-line choice due to its higher cost and a lack of clear superiority over other antibiotics.[1][15] Topical dapsone is sometimes a preferred therapy in women or for people with sensitive or darker-toned skin.[15] It is not recommended for use with benzoyl peroxide due to the risk of causing yellow-orange skin discoloration with this combination.[10] Minocycline is an effective acne treatment, but it is not a first-line antibiotic due to a lack of evidence that it is better than other treatments, and concerns about its safety compared to other tetracyclines.[108]
Sarecycline is the most recent oral antibiotic developed specifically for the treatment of acne, and is FDA-approved for the treatment of moderate to severe inflammatory acne in patients nine years of age and older.[109][110][111] It is a narrow-spectrum tetracycline antibiotic that exhibits the necessary antibacterial activity against pathogens related to acne vulgaris and a low propensity for inducing antibiotic resistance.[112][113] In clinical trials, sarecycline demonstrated clinical efficacy in reducing inflammatory acne lesions as early as three weeks and reduced truncal (back and chest) acne.[111][114]
Hormonal agents
In women, the use of
Pregnant and lactating women should not receive antiandrogens for their acne due to a possibility of
Hormonal treatments for acne such as combined birth control pills and antiandrogens may be considered first-line therapy for acne under many circumstances, including desired contraception, known or suspected hyperandrogenism, acne during adulthood, acne that flares premenstrually, and when symptoms of significant sebum production (seborrhea) are co-present.[164] Hormone therapy is effective for acne both in women with hyperandrogenism and in women with normal androgen levels.[164]
Azelaic acid
This section appears to contradict itself on efficacy. (December 2023) |
Salicylic acid
Other medications
Topical and oral preparations of
Combination therapy
Combination therapy—using medications of different classes together, each with a different mechanism of action—has been demonstrated to be a more effective approach to acne treatment than monotherapy.[10][50] The use of topical benzoyl peroxide and antibiotics together is more effective than antibiotics alone.[10] Similarly, using a topical retinoid with an antibiotic clears acne lesions faster than the use of antibiotics alone.[10] Frequently used combinations include the following: antibiotic and benzoyl peroxide, antibiotic and topical retinoid, or topical retinoid and benzoyl peroxide.[50] Dermatologists generally prefer combining benzoyl peroxide with a retinoid over the combination of a topical antibiotic with a retinoid. Both regimens are effective, but benzoyl peroxide does not lead to antibiotic resistance.[10]
Pregnancy
Although sebaceous gland activity in the skin increases during the late stages of pregnancy, pregnancy has not been reliably associated with worsened acne severity.
Topical antibiotics deemed safe during pregnancy include clindamycin, erythromycin, and metronidazole (all category B), due to negligible systemic absorption.[50][176] Nadifloxacin and dapsone (category C) are other topical antibiotics that may be used to treat acne in pregnant women but have received less study.[50][176] No adverse fetal events have been reported from the topical use of dapsone.[176] If retinoids are used there is a high risk of abnormalities occurring in the developing fetus; women of childbearing age are therefore required to use effective birth control if retinoids are used to treat acne.[20] Oral antibiotics deemed safe for pregnancy (all category B) include azithromycin, cephalosporins, and penicillins.[176] Tetracyclines (category D) are contraindicated during pregnancy as they are known to deposit in developing fetal teeth, resulting in yellow discoloration and thinned tooth enamel.[1][176] Their use during pregnancy has been associated with the development of acute fatty liver of pregnancy and is further avoided for this reason.[176]
Procedures
Limited evidence supports
When regular light is used immediately following the application of a
Dermal or subcutaneous
Alternative medicine
Researchers are investigating complementary therapies as treatment for people with acne.
Self-care
Many over-the-counter treatments in many forms are available, which are often known as
Prognosis
Acne usually improves around the age of 20 but may persist into adulthood.
Mental health impact
There is good evidence to support the idea that acne and associated scarring negatively affect a person's psychological state, worsen mood, lower self-esteem, and are associated with a higher risk of
Misperceptions about acne's causative and aggravating factors are common, and people with acne often blame themselves, and others often blame those with acne for their condition.[197][82] Such blame can worsen the affected person's sense of self-esteem.[197] Until the 20th century, even among dermatologists, the list of causes was believed to include excessive sexual thoughts and masturbation.[198] Dermatology's association with sexually transmitted infections, especially syphilis, contributed to the stigma.[198]
Another
Epidemiology
Globally, acne affects approximately 650 million people, or about 9.4% of the population, as of 2010.[200] It affects nearly 90% of people in Western societies during their teenage years, but can occur before adolescence and may persist into adulthood.[19][20][23] While acne that first develops between the ages of 21 and 25 is uncommon, it affects 54% of women and 40% of men older than 25 years of age[50][201] and has a lifetime prevalence of 85%.[50] About 20% of those affected have moderate or severe cases.[2] It is slightly more common in females than males (9.8% versus 9.0%).[200] In those over 40 years old, 1% of males and 5% of females still have problems.[20]
Rates appear to be lower in rural societies.[22] While some research has found it affects people of all ethnic groups,[202] acne may not occur in the non-Westernized peoples of Papua New Guinea and Paraguay.[203]
Acne affects 40–50 million people in the United States (16%) and approximately 3–5 million in Australia (23%).[125][204] Severe acne tends to be more common in people of Caucasian or Amerindian descent than in people of African descent.[21]
History
Historical records indicate Pharaohs had acne, which may be the earliest known reference to the disease. Sulfur's usefulness as a topical remedy for acne dates back to at least the reign of Cleopatra (69–30 BCE).[205] The sixth-century Greek physician Aëtius of Amida reportedly coined the term "ionthos" (ίονθωξ,) or "acnae", which seems to be a reference to facial skin lesions that occur during "the 'acme' of life" (puberty).[206]
In the 16th century, the French physician and botanist
The recognition and characterization of acne progressed in 1776 when
Scientists initially hypothesized that acne represented a disease of the skin's hair follicle, and occurred due to blockage of the pore by sebum. During the 1880s, they observed bacteria by microscopy in skin samples from people with acne. Investigators believed the bacteria caused comedones, sebum production, and ultimately acne.[206] During the mid-twentieth century, dermatologists realized that no single hypothesized factor (sebum, bacteria, or excess keratin) fully accounted for the disease in its entirety.[206] This led to the current understanding that acne could be explained by a sequence of related events, beginning with blockage of the skin follicle by excessive dead skin cells, followed by bacterial invasion of the hair follicle pore, changes in sebum production, and inflammation.[206]
The approach to acne treatment underwent significant changes during the twentieth century. Retinoids became a medical treatment for acne in 1943.[97] Benzoyl peroxide was first proposed as a treatment in 1958 and remains a staple of acne treatment.[209] The introduction of oral tetracycline antibiotics (such as minocycline) modified acne treatment in the 1950s. These reinforced the idea amongst dermatologists that bacterial growth on the skin plays an important role in causing acne.[206] Subsequently, in the 1970s, tretinoin (original trade name Retin A) was found to be an effective treatment.[210] The development of oral isotretinoin (sold as Accutane and Roaccutane) followed in 1980.[211] After its introduction in the United States, scientists identified isotretinoin as a medication highly likely to cause birth defects if taken during pregnancy. In the United States, more than 2,000 women became pregnant while taking isotretinoin between 1982 and 2003, with most pregnancies ending in abortion or miscarriage. Approximately 160 babies were born with birth defects due to maternal use of isotretinoin during pregnancy.[212][213]
Treatment of acne with topical crushed dry ice, known as cryoslush, was first described in 1907 but is no longer performed commonly.[214] Before 1960, the use of X-rays was also a common treatment.[215][216]
Society and culture
The costs and social impact of acne are substantial. In the United States, acne vulgaris is responsible for more than 5 million doctor visits and costs over US$2.5 billion each year in direct costs.[13] Similarly, acne vulgaris is responsible for 3.5 million doctor visits each year in the United Kingdom.[20] Sales for the top ten leading acne treatment brands in the US in 2015 amounted to $352 million.[217]
Acne vulgaris and its resultant scars are associated with significant social and academic difficulties that can last into adulthood.[31][218] During the Great Depression, dermatologists discovered that young men with acne had difficulty obtaining jobs.[198] Until the 1930s, many people viewed acne as a trivial problem among middle-class girls because, unlike smallpox and tuberculosis, no one died from it, and a feminine problem, because boys were much less likely to seek medical assistance for it.[198] During World War II, some soldiers in tropical climates developed such severe and widespread tropical acne on their bodies that they were declared medically unfit for duty.[198]
Research
Efforts to better understand the mechanisms of sebum production are underway. This research aims to develop medications that target and interfere with the hormones that are known to increase sebum production (e.g.,
The use of antimicrobial peptides against C. acnes is under investigation as a treatment for acne to overcoming antibiotic resistance.[10] In 2007, scientists reported the first genome sequencing of a C. acnes bacteriophage (PA6). The authors proposed applying this research toward the development of bacteriophage therapy as an acne treatment to overcome the problems associated with long-term antibiotic use, such as bacterial resistance.[219] Oral and topical probiotics are under evaluation as treatments for acne.[220] Probiotics may have therapeutic effects for those affected by acne due to their ability to decrease skin inflammation and improve skin moisture by increasing the skin's ceramide content.[220] As of 2014, knowledge of the effects of probiotics on acne in humans was limited.[220]
Decreased levels of retinoic acid in the skin may contribute to comedo formation. Researchers are investigating methods to increase the skin's production of retinoic acid to address this deficiency.[10] A vaccine against inflammatory acne has shown promising results in mice and humans.[53][221] Some have voiced concerns about creating a vaccine designed to neutralize a stable community of normal skin bacteria that is known to protect the skin from colonization by more harmful microorganisms.[222]
Other animals
Acne can occur on cats,[223] dogs,[224] and horses.[225][226]
References
- ^ PMID 26476248.
- ^ S2CID 24002879.
- ^ PMID 22284143.
- ^ PMID 16820822.
- ^ PMID 15814882.
- ISBN 9780781770354. Archivedfrom the original on 6 September 2017.
- ^ PMID 24719062.
- ^ PMID 23062156.
- ^ PMID 27733282.
- ^ S2CID 12685388.(subscription required)
- S2CID 44167421.
- ^ a b "Frequently Asked Questions: Acne" (PDF). U.S. Department of Health and Human Services, Office of Public Health and Science, Office on Women's Health. July 2009. Archived from the original (PDF) on 10 December 2016. Retrieved 30 July 2009.
- ^ PMID 22117871.
- ^ PMID 21909065.
- ^ S2CID 52914179.
- ^ S2CID 26027411.
- ^ S2CID 635373.
- PMID 24166134.
- ^ S2CID 7128254.
- ^ S2CID 5331094.
- ^ ISBN 978-1-84076-150-4. Archivedfrom the original on 2 July 2016.
- ^ S2CID 16534829.
- ^ S2CID 30549586.
- ^ ""acne", "vulgar"". Oxford English Dictionary (CD-ROM) (2nd ed.). Oxford: Oxford University Press. 2009.
- ^ ISBN 978-0-07-171755-7.
- ^ PMID 24767187.
- S2CID 5205305.
- ^ PMID 24314375.
- PMID 19439902.
- ^ PMID 22374611.
- ^ PMID 27015781.
- ^ S2CID 41448330.
- ^ PMID 25597636.
- S2CID 28374672.
- S2CID 240355253.
- ^ "International Consensus Recommend Acne Scar Treatments". Dermatology Times. 24 November 2021. Retrieved 28 November 2021.
- ^ PMID 22002814.
- ^ S2CID 43211448.
- ^ S2CID 9997519.
- PMID 35309879.
- ISBN 978-3-540-69374-1.
- ^ InformedHealth.org (26 September 2019). Acne: Overview. Institute for Quality and Efficiency in Health Care.
- PMID 24498378.
- ^ ISBN 978-0071440196.
- ISBN 978-1-4443-4536-0.
- ISBN 978-1-61631-009-7. Archivedfrom the original on 9 December 2016.
- ISBN 978-3-540-69375-8. Archivedfrom the original on 10 December 2016.
- ^ S2CID 28243535.
- ^ PMID 25437977.
- ^ S2CID 45531743.
- S2CID 13382470.
- PMID 26074745.
- ^ S2CID 37750291.
- ^ S2CID 29010884.
- ^ PMID 25454036.
- PMID 23975508.
- ^ PMID 20082944.
- ^ from the original on 21 February 2015.
- S2CID 25852903.
- S2CID 21580128.
- PMID 25441469.
- ^ PMID 25455069.
- ^ Garrick N (1 September 2016). "Acne". National Institute of Arthritis and Musculoskeletal and Skin Diseases.
- PMID 24187141.
- S2CID 25658207.
- PMID 25607703.
- ^ PMID 25465857.
- ^ S2CID 8848543.
- ISBN 978-0-632-06429-8.
- S2CID 162170301.
- ^ PMID 23972509.
- ^ S2CID 2296120.
- ^ O' Brien SC, Lewis JB, Cunliffe WJ. "The Leeds Revised Acne Grading System" (PDF). The Leeds Teaching Hospitals. Archived from the original (PDF) on 25 November 2015. Retrieved 23 November 2015.
- PMID 19450306.
- PMID 27015783.
- S2CID 33276273.
- ISBN 978-3-662-07677-4. Archivedfrom the original on 6 September 2017.
- ^ PMID 19507372.
- ^ S2CID 12200694.
- ^ PMID 26897386.
- PMID 31712293.
- ^ S2CID 240655201.
- PMID 33526498.
- ^ PMID 24688622.
- PMID 28210396.
- PMID 23322028.
- PMID 29104722.
- S2CID 9077120.
- S2CID 25191984.
- S2CID 44158118.
- ^ "Medical nutrition therapy shows positive benefits in dermatologic conditions". www.healio.com. Retrieved 10 March 2021.
- S2CID 12894377.
- ^ S2CID 5838346.
- PMID 32175593.
- ^ S2CID 26069784.
- S2CID 7912384.
- ^ S2CID 12663356.
- ^ "Drug Trials Snapshots: Aklief". U.S. Food and Drug Administration (FDA). 11 October 2019. Archived from the original on 19 November 2019. Retrieved 18 November 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "Isotretinoin". Drugs.com. Retrieved 25 April 2021.
- ^ S2CID 43870491.
- ^ "Arazlo lotion launched in US for acne treatment". Healio.com. Retrieved 10 March 2021.
- PMID 30484286.
- ^ PMID 27015777.
- PMID 24147278.
- ^ (PDF) from the original on 5 November 2018. Retrieved 1 January 2019.
- ^ PMID 30296534.
- ^ Hilton L (21 March 2019). "Dermatologists relying less on antibiotics for acne". Dermatology Times. Archived from the original on 7 June 2020. Retrieved 7 June 2020.
- PMID 22895927.
- ^ "Prescribing Information for Seysara" (PDF).
{{cite journal}}: Cite journal requires|journal=(help) - PMID 29537451.
- ^ PMID 31475868.
- ^ "Sarecycline". PubChem. U.S. National Library of Medicine. Retrieved 7 June 2020.
- PMID 30397052.
- PMID 30235387.
- PMID 22786490.
- ^ ISBN 978-3-642-64261-6.
- ^ S2CID 5777817.
- (PDF) from the original on 22 August 2016. Retrieved 21 December 2018.
- S2CID 10136018.
- S2CID 43381309.
- S2CID 71806394.
- PMID 22786490.
- PMID 28292450.
- PMID 29725277.
- ^ PMID 24880665.
- ^ PMID 28155090.
- S2CID 258717921.
- ^ S2CID 35615492.
- S2CID 46484837.
- ^ PMID 6235105.
- ^ ISBN 9780120405213.
- PMID 19297634.
- ^ S2CID 52973096.
- S2CID 37512606.
- ^ "FDA. Prescribing Information" (PDF).
- PMID 30467659.
- PMID 28979664.
- S2CID 220924754.
- ^ hdl:11573/1492686.
- PMID 32419942.
- ^ PMID 33536184.
- S2CID 220720801.
- S2CID 2628354.
- S2CID 4640778.
- ^ from the original on 27 February 2020. Retrieved 21 December 2018.
- ISBN 978-0-7216-8258-7.
- ISBN 978-1-906985-41-7.
- ^ PMID 28492054.
- ^ PMID 28379593.
- .
- PMID 28274354.
- PMID 8717470.
- S2CID 34153031.
- PMID 27416311.
- ^ "Winlevi (clascoterone) cream, for topical use" (PDF). Cassiopea. Retrieved 9 September 2020.
- S2CID 53718051.
- .
- ^ S2CID 4398912.
- ^ PMID 29872679.
- ^ S2CID 12685388.
- ^ PMID 23377402.
- ^ ISBN 978-1-118-23277-4.
- S2CID 8325257.
- ^ PMID 20082945.
- ^ S2CID 5750718.
- S2CID 58809558.
- PMID 18246693.
- PMID 20493337.
- ^ MedlinePlus Encyclopedia: Azelaic Acid Topical
- PMID 32356369.
- ^ PMID 24472429.
- PMID 24048347.
- ^ S2CID 28160151.
- ^ PMID 23652948.
- PMID 27015774.
- ^ S2CID 31034803.
- ^ S2CID 41362332.
- S2CID 13637965.
- ISBN 9780702051821.
- PMID 29541753.
- S2CID 6902995.
- PMID 27670126.
- ^ PMID 26549251.
- S2CID 205262673.
- PMID 27038134.
- ^ from the original on 19 September 2018. Retrieved 19 September 2018.
- PMID 22587597.
- PMID 26057505.
- PMID 28095556.
- S2CID 25638674.
- ^ PMID 25597924.
- S2CID 10111211.
- PMID 22808307.
- ^ S2CID 36792285.
- ISBN 978-0323054058. Archivedfrom the original on 6 September 2017.
- ISBN 9781437703146.
- ^ PMID 16894437.
- ^ ISBN 9780307755742. Archivedfrom the original on 12 March 2017.
- ISBN 978-0-323-31956-0. Archivedfrom the original on 6 September 2017.
- ^ PMID 23245607.
- S2CID 40314598.
- S2CID 27893826.
- S2CID 19433549.
- PMID 9703121.
- PMID 21436973.
- ^ S2CID 32660371.
- ISBN 9780702051821.
- ^ Bulkley LD (1885). Acne; Its Etiology, Pathology and Treatment. New York: G.P. Putnam's Sons. Archived from the original on 5 May 2016. Retrieved 15 February 2020.
- from the original on 27 February 2017.
- PMID 4265099.
- S2CID 40877032.
- PMID 17214828.
- S2CID 46287015.
- PMID 20468218.
- PMID 20769902.
- .
- ^ "Sales of the leading acne brands in the United States in 2015 (in million U.S. dollars)". statista: The Statistics Portal. Statista Inc. Archived from the original on 12 March 2017. Retrieved 12 March 2017.
- PMID 23557650.
- PMID 17400737.
- ^ PMID 24906613.
- PMID 26264195.
- ^ MacKenzie D. "In development: a vaccine for acne". New Scientist. Archived from the original on 2 April 2015. Retrieved 30 March 2015.
- PMID 34644839.
- ^ Veterinary Medicine. 1914. Archived from the original on 12 March 2017.
- ISBN 9780702039911. Archivedfrom the original on 12 March 2017.
- ^ White DS (1917). A Text-book of the Principles and Practice of Veterinary Medicine. Lea & Febiger. p. 258.
Further reading
- Paller AS, Mancini AJ (2015). Hurwitz's Clinical Pediatric Dermatology: A Textbook of Skin Disorders of Childhood And Adolescence. Elsevier. ISBN 978-0-323-24475-6.
- Cordain L, Lindeberg S, Hurtado M, Hill K, Eaton SB, Brand-Miller J (December 2002). "Acne vulgaris: a disease of Western civilization". Archives of Dermatology. 138 (12): 1584–90. PMID 12472346.
- Del Rosso JQ (December 2013). "The role of skin care as an integral component in the management of acne vulgaris: part 1: the importance of cleanser and moisturizer ingredients, design, and product selection". The Journal of Clinical and Aesthetic Dermatology. 6 (12): 19–27. PMID 24765221.
- "Acne". MedlinePlus. U.S. National Library of Medicine.
External links
- Acne Support. Expert, impartial advice on acne by the British Association of Dermatologists (BAD).



