Causes of cancer
Cancer is caused by
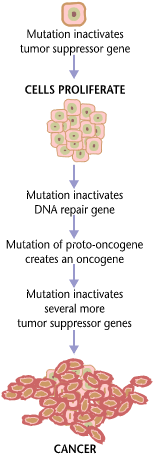
Over one third of cancer deaths worldwide (and about 75–80% in the United States) are potentially avoidable by reducing exposure to known factors.[7][8] Common environmental factors that contribute to cancer death include exposure to different chemical and physical agents (tobacco use accounts for 25–30% of cancer deaths), environmental pollutants, diet and obesity (30–35%), infections (15–20%), and radiation (both ionizing and non-ionizing, up to 10%).[9] These factors act, at least partly, by altering the function of genes within cells.[10] Typically many such genetic changes are required before cancer develops.[10] Aging has been repeatedly and consistently regarded as an important aspect to consider when evaluating the risk factors for the development of particular cancers. Many molecular and cellular changes involved in the development of cancer accumulate during the aging process and eventually manifest as cancer.[11]
Genetics

Although there are over 50 identifiable hereditary forms of cancer, less than 0.3% of the population are carriers of a cancer-related genetic mutation and these make up less than 3–10% of all cancer cases.
Many of the cancer syndrome cases are caused by mutations in
Gene mutations are classified as germline or somatic depending on the cell type where they appear (germline cells include the egg and the sperm and somatic cells are those forming the body). The germline mutations are carried through generations and increase the risk of cancer.[citation needed]
Cancer syndromes
- Ataxia–telangiectasia
- Bloom syndrome
- BRCA1 & BRCA2
- Fanconi anemia
- Familial adenomatous polyposis
- Hereditary breast and ovarian cancer
- Hereditary nonpolyposis colorectal cancer
- Li–Fraumeni syndrome
- Nevoid basal-cell carcinoma syndrome
- Von Hippel–Lindau disease
- Werner syndrome
- Xeroderma pigmentosum
Physical and chemical agents
Particular substances, known as
Smoking


Electronic cigarettes or
Materials
Lifestyle
Many different lifestyle factors contribute to increasing cancer risk. Together, diet and obesity are related to approximately 30–35% of cancer deaths.[9][34] Dietary recommendations for cancer prevention typically include an emphasis on vegetables, fruit, whole grains, and fish, and avoidance of processed meat, red meat, animal fats, and refined carbohydrates.[35] The evidence to support these dietary changes is not definitive.[36]
Alcohol
Diet
Some specific foods have been linked to specific cancers.
The relationship between diet and the development of particular cancers may partly explain differences in cancer incidence in different countries. For example,
When
Obesity
| Men | Women |
|---|---|
| Colorectal cancer | Colorectal cancer |
Esophageal adenocarcinoma
|
Endometrial cancer |
| Kidney cancer | Esophageal adenocarcinoma
|
| Pancreatic cancer | Gallbladder cancer |
| Thyroid cancer | Kidney cancer |
| Pancreatic cancer | |
| Post-menopausal breast cancer |
In the United States, excess body weight is associated with the development of many types of cancer and is a factor in 14–20% of all cancer deaths.[34] Every year, nearly 85,000 new cancer diagnoses in the United States are related to obesity.[54] Individuals who underwent bariatric surgery for weight loss have reduced cancer incidence and mortality.[54]
There is an association between obesity and colon cancer, post-menopausal breast cancer, endometrial cancer, kidney cancer, and esophageal cancer.
Physical inactivity is believed to contribute to cancer risk not only through its effect on body weight but also through negative effects on immune system and endocrine system.[34] More than half of the effect from diet is due to overnutrition rather than from eating too little healthy foods.[54]
Hormones

Some hormones play a role in the development of cancer by promoting cell proliferation.[58] Insulin-like growth factors and their binding proteins play a key role in cancer cell growth, differentiation and apoptosis, suggesting possible involvement in carcinogenesis.[59]
Hormones are important agents in sex-related cancers such as cancer of the breast, endometrium, prostate, ovary, and testis, and also of
Other factors are also relevant: obese people have higher levels of some hormones associated with cancer and a higher rate of those cancers.
Some treatments and prevention approaches leverage this cause by artificially reducing hormone levels, and thus discouraging hormone-sensitive cancers. Because steroid hormones are powerful drivers of gene expression in certain cancer cells, changing the levels or activity of certain hormones can cause certain cancers to cease growing or even undergo cell death.
Infection and inflammation
Worldwide, approximately 18% of cancer cases are related to
Viruses

Viral infection is a major risk factor for cervical and liver cancer.
In Western developed countries, human papillomavirus (HPV), hepatitis B virus (HBV) and hepatitis C virus (HCV) are the most common oncoviruses.
Bacteria and parasites
Inflammation
There is evidence that inflammation itself plays an important role in the development and progression of cancer.[71] Chronic inflammation can lead to DNA damage over time and the accumulation of random genetic alterations in cancer cells.[72] Inflammation can contribute to proliferation, survival, angiogenesis and migration of cancer cells by influencing tumor microenvironment.[73] Individuals with inflammatory bowel disease are at increased risk of developing colorectal cancers.[13]
Radiation
Up to 10% of invasive cancers are related to radiation exposure, including both
Non-ionizing radiation
Higher-energy radiation, including
Ionizing radiation
Ionizing radiation is also used in some kinds of medical imaging. In industrialized countries, medical imaging contributes almost as much radiation dose to the public as natural background radiation. Nuclear medicine techniques involve the injection of radioactive pharmaceuticals directly into the bloodstream. Radiotherapy deliberately deliver high doses of radiation to tumors and surrounding tissues as a form of disease treatment. It is estimated that 0.4% of cancers in 2007 in the United States are due to CTs performed in the past and that this may increase to as high as 1.5–2% with rates of CT usage during this same time period.[80]
Residential exposure to radon gas has similar cancer risks as passive smoking.[74] Low-dose exposures, such as living near a nuclear power plant, are generally believed to have no or very little effect on cancer development.[74] Radiation is a more potent source of cancer when it is combined with other cancer-causing agents, such as radon gas exposure plus smoking tobacco.[74]
Rare causes
Organ transplantation

The development of donor-derived tumors from
Trauma
Maternal-fetal transmission
In the
References
- PMID 29570697.
- PMID 25869442.
- ^ S2CID 24746283.

- ISBN 978-9283204299.
- ^ Cancer and the Environment: What you Need to Know, What You Can Do. NIH Publication No. 03-2039: National Institutes of Health. 2003.
Cancer develops over several years and has many causes. Several factors both inside and outside the body contribute to the development of cancer. In this context, scientists refer to everything outside the body that interacts with humans as 'environmental'.
{{cite book}}: CS1 maint: location (link) - ISBN 978-0-387-78192-1 – via Open Library.
The term environment refers not only to air, water, and soil but also to substances and conditions at home and at the workplace, including diet, smoking, alcohol, drugs, exposure to chemicals, sunlight, ionizing radiation, electromagnetic fields, infectious agents, etc. Lifestyle, economic and behavioral factors are all aspects of our environment.
- PMID 7017215.
- PMID 27460784 – via ScienceDirect.
- ^ PMID 18626751.
- ^ ISBN 978-9283204299.
- ^ "Cancer Fact sheet N°297". World Health Organization. February 2014. Retrieved 10 June 2014.
- PMID 18196605.
- ^ ISBN 978-9283204299.
- PMID 10686303.
- ^ "National Institute for Occupational Safety and Health- Occupational Cancer". United States National Institute for Occupational Safety and Health. Retrieved 13 October 2007.
- ^ a b c "WHO calls for prevention of cancer through healthy workplaces" (Press release). World Health Organization. 27 April 2007. Archived from the original on 1 May 2007. Retrieved 13 October 2007.
- PMID 18055160.
- PMID 23393080.
- ^ "Share of cancer deaths attributed to tobacco". Our World in Data. Retrieved 5 March 2020.
- ^ PMID 15552776.
- S2CID 20891885.
- ^ S2CID 6132726.
- ^ Cunningham FH, Fiebelkorn S, Johnson M, Meredith C. A novel application of the Margin of Exposure approach: segregation of tobacco smoke toxicants. Food Chem Toxicol. 2011 Nov;49(11):2921-33. doi: 10.1016/j.fct.2011.07.019. Epub 2011 Jul 23. PMID 21802474
- ^ Pu X, Kamendulis LM, Klaunig JE. Acrylonitrile-induced oxidative stress and oxidative DNA damage in male Sprague-Dawley rats. Toxicol Sci. 2009;111(1):64-71. doi:10.1093/toxsci/kfp133
- ^ Li L, Jiang L, Geng C, Cao J, Zhong L. The role of oxidative stress in acrolein-induced DNA damage in HepG2 cells. Free Radic Res. 2008 Apr;42(4):354-61. doi: 10.1080/10715760802008114. PMID 18404534
- ^ S2CID 9172672.
- PMID 16998161.
- PMID 18434333.
- PMID 15217537.
- PMID 26164573.
- PMID 25572196.
- ^ ISBN 978-1-55009-113-7. Retrieved 31 January 2011.
- )
- ^ S2CID 19823935.
- S2CID 2067308.
- PMID 21904992.
- ^ "IARC: IARC Strengthens its Findings on Several Carcinogenic Personal Habits and Household Exposures" (PDF). International Agency for Research on Cancer - World Health Organization. 2009.
- PMID 21474525.
- S2CID 14938863.
- ^ "Alcohol Consumption and the Risk of Cancer". pubs.niaaa.nih.gov. Archived from the original on 21 February 2018. Retrieved 22 March 2018.
- PMID 15972793.
- ^ a b Hodskinson MR, Bolner A, Sato K, Kamimae-Lanning AN, Rooijers K, Witte M, Mahesh M, Silhan J, Petek M, Williams DM, Kind J, Chin JW, Patel KJ, Knipscheer P. Alcohol-derived DNA crosslinks are repaired by two distinct mechanisms. Nature. 2020 Mar;579(7800):603-608. doi: 10.1038/s41586-020-2059-5. Epub 2020 Mar 4. PMID 32132710; PMCID: PMC7116288.
- PMID 15082451.
- ISBN 9789283204299.
- PMID 20374790.
- ^ "Colorectal Cancer 2011 Report: Food, Nutrition, Physical Activity, and the Prevention of Colorectal Cancer" (PDF). World Cancer Research Fund & American Institute for Cancer Research. 2011. Archived from the original (PDF) on 22 May 2019. Retrieved 22 March 2018.
- PMID 18990005. Archived from the original(PDF) on 4 September 2011. Retrieved 17 July 2014.
- PMID 19107449.
- S2CID 39881987.
- PMID 9081351.
- ^ Prasad AR, Prasad S, Nguyen H, Facista A, Lewis C, Zaitlin B, et al. (July 2014). "Novel diet-related mouse model of colon cancer parallels human colon cancer". World Journal of Gastrointestinal Oncology. 6 (7): 225–43. doi:10.4251/wjgo.v6.i7.225. PMC 4092339. PMID 25024814
- PMID 21267546.
- ^ Erikka Loftfield, PhD, MPH, Roni T Falk, MS, Joshua N Sampson, PhD, Wen-Yi Huang, PhD, Autumn Hullings, MPH, Gwen Murphy, PhD, MPH, Stephanie J Weinstein, PhD, Demetrius Albanes, MD, Neal D Freedman, PhD, MPH, Rashmi Sinha, PhD, Prospective Associations of Circulating Bile Acids and Short-Chain Fatty Acids with Incident Colorectal Cancer, JNCI Cancer Spectrum, 2022;, pkac027, https://doi.org/10.1093/jncics/pkac027
- ^ PMID 21080117.
- PMID 24007864.
- PMID 23121183.
- ^ Kompella P, Vasquez KM. Obesity and cancer: A mechanistic overview of metabolic changes in obesity that impact genetic instability. Mol Carcinog. 2019 Sep;58(9):1531-1550. doi: 10.1002/mc.23048. Epub 2019 Jun 5. PMID 31168912; PMCID: PMC6692207
- ^ ISBN 978-1-55009-113-7. Retrieved 27 January 2011.
- PMID 19142965.
- PMID 22575588.
- S2CID 38402898.
- PMID 18626751.
- ^ "Human Papillomavirus (HPV) and Cancer". CDC. 2 January 2018. Retrieved 22 March 2018.
- PMID 15479788.
- ^ a b Sung MW, Thung SN, Acs G (2000). Hepatitis Viruses. BC Decker.
- PMID 15489139.
- PMID 16367902.
- PMID 20539059.
- ^ Mustacchi, Piero (2000). Parasites. BC Decker.
- PMID 23921082.
- PMID 24552665.
- PMID 19468060.
- PMID 20455855.
- ^ ISBN 978-1-55009-113-7.
- ^ "IARC classifies radiofrequency electromagnetic fields as possibly carcinogenic to humans" (PDF). World Health Organization.
- ^ "IARC Monographs- Classifications". monographs.iarc.fr. Archived from the original on 10 June 2017. Retrieved 13 March 2018.
- ^ "Cell Phones and Cancer Risk - National Cancer Institute". Cancer.gov. 8 May 2013. Retrieved 15 December 2013.
- ^ ISBN 978-1-55009-113-7. Retrieved 31 January 2011.
- PMID 27713063.
- S2CID 2760372.
- PMID 16957717.
- S2CID 2527251.
- ^ ISBN 978-1-55009-113-7. Retrieved 27 January 2011.
- ^ PMID 12794519.
