Discovery and development of direct thrombin inhibitors
Direct thrombin inhibitors (DTIs) are a class of
History

Mechanism of action
Blood clotting cascade

When a
Binding sites
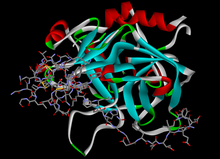
Thrombin is in the
DTIs inhibition

.
DTIs inhibit thrombin by two ways;
Active site's pockets

DTIs that fit in the active binding site have to fit in the hydrophobic pocket (S1) that contains aspartic acid residue at the bottom which recognizes the basic side chain. The S2 site has a loop around tryptophan which occludes a hydrophobic pocket that can recognize larger aliphatic residues. The S3 site is flat and the S4 site is hydrophobic, it has tryptophan lined by leucine and isoleucine.[9]

Nα-(2-naphthyl-sulphonyl-glycyl)-DL-p-amidinophenylalanyl-piperidine (NAPAP) binds thrombin in the S1, S2 and S4 pockets. The amidine group on NAPAP forms a bidentate salt bridge with Asp deep in the S1 pocket, the piperidine group takes the role of proline residue and binds in the S2 pocket, and the naphthyl rings of the molecule forms a hydrophobic interaction with Trp in the S4 pocket. Pharmaceutical companies have used the structural knowledge of NAPAP to develop DTIs. Dabigatran, like NAPAP binds to S1, S2 and S4 pockets. Benzamidine group on the dabigatran structure binds deep in the S1 pocket, the methylbenzimidazole fits nicely in the hydrophobic S2 pocket and the Ile and Leu at the bottom of the S4 pocket binds to the aromatic group of dabigatran.[9]
Drug development
Hirudin derivatives
Hirudin
Hirudin
In a
Lepirudin

Lepirudin is approved for the treatment of
Desirudin
Desirudin is approved for treatment of
Bivalirudin

Small molecular direct thrombin inhibitors
Small molecular direct thrombin inhibitors (smDTIs) are non-peptide small molecules that specifically and reversibly inhibit both free and clot-bound thrombin by binding to the active site of the thrombin molecule. They prevent VTE in patients undergoing hip- and knee replacement surgery.[10] The advantages of this type of DTIs are that they do not need monitoring, have a wide therapeutic index and the possibility of oral administration route. They are theoretically more convenient than both vitamin K antagonist and LMWH. Researches will, however, have to show the indication of the use and their safety.[18]
The smDTIs where derived using a peptidomimetic design with either P1 residue from arginine itself (e.g. argatroban) or arginine-like substrates such as benzamidine (e.g. NAPAP).[9]
Argatroban

Ximelagatran
The publication of the NAPAP-fIIa

Dabigatran etexilate
Researchers at
In a 2012 meta-analysis dabigatran was associated with increased risk of myocardial infarction (MI) or ACS when tested against different controls in a broad spectrum of patients.[22]

Table 1: Summary of characteristics of DTIs
| Bivalent/ Univalent[4] | Route of administration[10] | Metabolism[10] | Binding to active site and/or exosite 1[4] | Indications | Limitations | Advantages | |
| Native Hirudin | B | (Parenteral) | Has no indications | ||||
| Lepirudin | B | Parenteral (iv/sc) | Renal | Irreversible | Prevention of further thrombosis in patients with HIT[16] | Narrow TI, potential increased bleedings, antihirudid antibodies are formed in 40% of patients, need for weight-based dosing[10] | |
Desirudin |
B | Parenteral (iv/sc) | Renal | Irreversible | Europe: treatment of VTE[4] USA: Prevention of DVT in patients undergoing hip replacement surgery[23] | Less need for weight-based doses and routine monitoring compared to lepirudin because of sc administration[10] | |
| Bivalirudin | B | Parenteral (iv) | Proteolytic cleavage, hepatic, 20% renal | Reversible | Prevention of acute ischemic complications in patients with unstable angina and with or at risk of HIT undergoing PTCA or PCI[24] | Dose adjustments are needed in severe renal impairment[16] | Decreased bleeding risk due to reversible binding,[4] improved safety profile compared with r-hirudins, fast onset of action[10] |
| Argatroban | U | Parenteral (iv) | Hepatical, mostly biliary | Reversible | Prevention and treatment of thrombosis in patients with HIT[10] | No bolus dose needed[10] | |
| Ximelagatran | U | Oral | Hepatic | Reversible | Europe: Prevention of VTE[10]
USA: FDA never gave approval[20] |
Long-term therapy (›35 days) is associated to hepatotoxicity – taken off market in Europe[18] | |
Dabigatran etexilate |
U | Oral | Primarily renal, remainder is conjugated with glucuronic acid in liver | Reversible | Prevention of stroke and embolism in patients with AF[25] | Rapid onset of action, lack of interaction with CYP450, food or drugs, broad TI, fixed dose administration and good safety profile, not associated with hepatotoxicity for long-term use[10] |
iv: intravenous, sc: subcutaneous, HIT: heparin-induced thrombocytopenia, VTE: Venous thromboembolism, DVT: Deep vein thrombosis, PTCA: Percutaneous transluminal coronary angioplasty, PCI: percutaneous coronary intervention, FDA: Food and Drug Administration, AF: Atrial fibrillation, TI: Therapeutic index
Status 2014
In 2014 dabigatran remains the only approved oral DTI
See also
- Anticoagulation
- Dabigatran
- Bivalirudin
- Warfarin
- Heparin
References
- S2CID 24817396.
- PMID 15013545.
- ^ PMID 14585945.
- ^ S2CID 6771526.
- PMID 15383472.
- ^ S2CID 3665578.
- PMID 22276081.
- ^ PMID 16148288.
- ^ PMID 22503439.
- ^ PMID 21241354.
- PMID 8145785. WOS:A1994NJ51200008.
- ^ PMID 8087958.
- ISBN 978-0-19-956908-3.)
{{cite book}}:|first=has generic name (help)CS1 maint: multiple names: authors list (link - ^ PMID 12356489.
- ^ PMID 18449411.
- ^ PMID 21457505.
- ^ "Lepirudin Injection". American Society of Health-System Pharmacists. Retrieved 18 September 2012.
- ^ S2CID 25332427.
- ^ PMID 15692265.
- ^ a b heartwire. "FDA opts not to approve ximelagatran". Retrieved 19 September 2012.
- PMID 11960487.
- PMID 22231617.
- ^ "Iprivask 15 mg" (PDF). Retrieved 18 September 2012.
- ^ "Angiomax Injection" (PDF). Food and Drug Administration. Retrieved 18 September 2012.
- ^ "FDA approves Pradaxa to prevent stroke in people with atrial fibrillation". Food and Drug Administration. Retrieved 18 September 2012.
- ^ PMID 22742650.
- ^ "AZD0837". Astrazenecaclinicaltrials.com. Retrieved 2012-10-16.
- ^ AstraZeneca Long-term treatment with the oral direct thrombin inhibitor AZD0837, compared to Vitamin-K antagonists, as stroke prevention in patients with non-valvular atrial fibrillation and one or more risk factors for stroke and systemic embolic events. A 5-year follow-up study study code D1250C0004221 January 2010 Trial D1250C00042 Archived November 10, 2013, at the Wayback Machine
- PMID 20368532.
- PMID 19690349.
