Warfarin
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˈwɔːrfərɪn/ |
| Trade names | Coumadin, others[1][2][3] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682277 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth, intravenous |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 79–100% (by mouth)[7] |
| Protein binding | 99%[8] |
| Metabolism | Liver: CYP2C9, 2C19, 2C8, 2C18, 1A2 and 3A4[8] |
| Elimination half-life | 1 week (active half-life is 20-60 hours)[8] |
| Excretion | Kidney (92%)[8] |
| Identifiers | |
| |
JSmol) | |
| |
| |
| | |
Warfarin is an
The common
Warfarin decreases blood clotting by blocking
Warfarin first came into large-scale commercial use in 1948 as a
Medical uses
Warfarin is used to decrease the tendency for
Warfarin is best suited for anticoagulation (clot formation inhibition) in areas of slowly running blood (such as in veins and the pooled blood behind artificial and natural valves), and in blood pooled in dysfunctional
Dosing
Dosing of warfarin is complicated because it is known to interact with many commonly used medications and
Maintenance dose
Recommendations by many national bodies, including the American College of Chest Physicians,[29] have been distilled to help manage dose adjustments.[30]
The
Several studies reported that the maintenance dose can be predicted based on various clinical data.[32][33]
Self-testing

Anticoagulation with warfarin can also be monitored by patients at home. International guidelines on home testing were published in 2005.[34] The guidelines stated:[34]
The consensus agrees that patient self-testing and patient self-management are effective methods of monitoring oral anticoagulation therapy, providing outcomes at least as good as, and possibly better than, those achieved with an anticoagulation clinic. All patients must be appropriately selected and trained. Currently available self-testing/self-management devices give INR results that are comparable with those obtained in laboratory testing.
A 2006
Alternative anticoagulants
In some countries, other
Contraindications
All anticoagulants are generally contraindicated in situations in which the reduction in clotting that they cause might lead to serious and potentially life-threatening bleeds. This includes people with active bleeding conditions (such as
Warfarin should not be given to people with
Pregnancy
Warfarin is
First trimester of pregnancy
Usually, warfarin is avoided in the
When warfarin (or another 4-hydroxycoumarin derivative) is given during the first trimester—particularly between the sixth and ninth weeks of pregnancy—a constellation of birth defects known variously as
Second trimester and later
Warfarin administration in the second and third trimesters is much less commonly associated with birth defects, and when they do occur, are considerably different from FWS. The most common congenital abnormalities associated with warfarin use in late pregnancy are central nervous system disorders, including spasticity and seizures, and eye defects.[41][42] Because of such later pregnancy birth defects, anticoagulation with warfarin poses a problem in pregnant women requiring warfarin for vital indications, such as stroke prevention in those with artificial heart valves.
Warfarin may be used in
Adverse effects
Bleeding
The only common side effect of warfarin is hemorrhage. The risk of severe bleeding is small but definite (a typical yearly rate of 1–3% has been reported),
Several risk scores exist to predict bleeding in people using warfarin and similar anticoagulants. A commonly used score (
Warfarin necrosis
A rare but serious complication resulting from treatment with warfarin is
Osteoporosis
After initial reports that warfarin could reduce
A 2006 retrospective study of 14,564 Medicare recipients showed that warfarin use for more than one year was linked with a 60% increased risk of osteoporosis-related fracture in men, but no association in women was seen. The mechanism was thought to be a combination of reduced intake of vitamin K (a vitamin necessary for bone health) and inhibition by warfarin of vitamin K-mediated carboxylation of certain bone proteins, rendering them nonfunctional.[54]
Purple toe syndrome
Another rare complication that may occur early during warfarin treatment (usually within 3 to 8 weeks of commencement) is purple toe syndrome. This condition is thought to result from small deposits of cholesterol breaking loose and causing embolisms in blood vessels in the skin of the feet, which causes a blueish-purple colour and may be painful.[55]
It is typically thought to affect the
Calcification
Several studies have also implicated warfarin use in valvular and vascular calcification. No specific treatment is available, but some modalities are under investigation.[57]
Overdose
The major side effect of warfarin use is bleeding. Risk of bleeding is increased if the INR is out of range (due to accidental or deliberate overdose or due to interactions).[44] Many drug interactions can increase the effect of warfarin, also causing an overdose.[26]
In patients with supratherapeutic INR but INR less than 10 and no bleeding, it is enough to lower the dose or omit a dose, monitor the INR and resume warfarin at an adjusted lower dose when the target INR is reached.
When warfarin is being given and INR is in therapeutic range, simple discontinuation of the drug for five days is usually enough to reverse the effect and cause INR to drop below 1.5.[61]
| Supratherapeutic INR but INR < 4.5, no bleeding |
|
|---|---|
| INR 4.5-10, no bleeding |
|
| INR >10.0, no bleeding |
|
| Minor bleeding, any elevated INR: |
|
| Major bleeding, any elevated INR |
May also consider supplementation with fresh frozen plasma (FFP) or recombinant factor VIIa |
| Life-threatening bleeding and elevated INR: |
|
Interactions
Warfarin
When taken with
Many commonly used
Excessive use of alcohol is also known to affect the metabolism of warfarin and can elevate the INR, and thus increase the risk of bleeding.[70] The U.S. Food and Drug Administration (FDA) product insert on warfarin states that alcohol should be avoided.[8] The Cleveland Clinic suggests that when taking warfarin one should not drink more than "one beer, 6 oz of wine, or one shot of alcohol per day".[71]
Warfarin also interacts with many herbs and spices,
Between 2003 and 2004, the UK Committee on Safety of Medicines received several reports of increased INR and risk of haemorrhage in people taking warfarin and cranberry juice.[75][76][77] Data establishing a causal relationship are still lacking, and a 2006 review found no cases of this interaction reported to the USFDA;[77] nevertheless, several authors have recommended that both doctors and patients be made aware of its possibility.[78] The mechanism behind the interaction is still unclear.[77]
Chemistry

X-ray
Stereochemistry
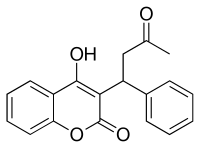
Warfarin contains a
| Enantiomers of warfarin | |
|---|---|
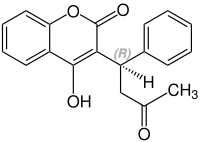 CAS Number: 5543-58-8 |
 CAS Number: 5543-57-7 |
Pharmacology

Pharmacokinetics
Warfarin consists of a
Warfarin is slower-acting than the common anticoagulant heparin, though it has a number of advantages. Heparin must be given by injection, whereas warfarin is available orally. Warfarin has a long half-life and need only be given once a day. Heparin can also cause a prothrombotic condition, heparin-induced thrombocytopenia (an antibody-mediated decrease in platelet levels), which increases the risk for thrombosis. It takes several days for warfarin to reach the therapeutic effect, since the circulating coagulation factors are not affected by the drug (thrombin has a half-life time of days). Warfarin's long half-life means that it remains effective for several days after it is stopped. Furthermore, if given initially without additional anticoagulant cover, it can increase thrombosis risk (see below).
Mechanism of action
Warfarin is one of several drugs often referred to as a "blood thinner"; this is not technically correct, as these drugs reduce coagulation of blood, increasing the clotting time, without affecting the viscosity ("thickness") as such of blood.[83]
Warfarin inhibits the vitamin K-dependent synthesis of biologically active forms of the
When warfarin is newly started, it may promote clot formation temporarily, because the level of proteins C and S are also dependent on vitamin K activity. Warfarin causes decline in protein C levels in first 36 hours. In addition, reduced levels of protein S lead to a reduction in activity of protein C (for which it is the co-factor), so reduces degradation of factor Va and factor VIIIa. Although loading doses of warfarin over 5 mg also produce a precipitous decline in factor VII, resulting in an initial prolongation of the INR, full antithrombotic effect does not take place until significant reduction in factor II occurs days later. The haemostasis system becomes temporarily biased towards thrombus formation, leading to a prothrombotic state. Thus, when warfarin is loaded rapidly at greater than 5 mg per day, to co-administering heparin, an anticoagulant that acts upon antithrombin and helps reduce the risk of thrombosis, is beneficial, with warfarin therapy for four to five days, to have the benefit of anticoagulation from heparin until the full effect of warfarin has been achieved.[89][90]
Pharmacogenomics
Warfarin activity is determined partially by genetic factors. Polymorphisms in two genes (VKORC1 and CYP2C9) play a particularly large role in response to warfarin.
VKORC1 polymorphisms explain 30% of the dose variation between patients:[91] particular mutations make VKORC1 less susceptible to suppression by warfarin.[88] There are two main haplotypes that explain 25% of variation: low-dose haplotype group (A) and a high-dose haplotype group (B).[92] VKORC1 polymorphisms explain why African Americans are on average relatively resistant to warfarin (higher proportion of group B haplotypes), while Asian Americans are generally more sensitive (higher proportion of group A haplotypes).[92] Group A VKORC1 polymorphisms lead to a more rapid achievement of a therapeutic INR, but also a shorter time to reach an INR over 4, which is associated with bleeding.[93]
Despite the promise of
History
In the early 1920s, an outbreak occurred of a previously unrecognized cattle disease in the
In 1921,
The identity of the anticoagulant substance in spoiled sweet clover remained a mystery until 1940. In 1933, Karl Paul Link and his laboratory of chemists working at the University of Wisconsin set out to isolate and characterize the haemorrhagic agent from the spoiled hay.[97] Five years were needed before Link's student, Harold A. Campbell, recovered 6 mg of crystalline anticoagulant. Next, Link's student, Mark A. Stahmann, took over the project and initiated a large-scale extraction, isolating 1.8 g of recrystallized anticoagulant in about 4 months. This was enough material for Stahmann and Charles F. Huebner to check their results against Campbell's, and to thoroughly characterize the compound. Through degradation experiments, they established that the anticoagulant was 3,3'-methylenebis-(4-hydroxycoumarin), which they later named dicoumarol. They confirmed their results by synthesizing dicoumarol and proving in 1940 that it was identical to the naturally occurring agent.[101]
Dicoumarol was a product of the plant molecule
Over the next few years, numerous similar chemicals (specifically 4-hydroxycoumarins with a large
After an incident in 1951, in which an army inductee attempted suicide with multiple doses of warfarin in rodenticide, but recovered fully after presenting to a naval hospital and being treated with vitamin K (by then known as a specific
The exact mechanism of action remained unknown until it was demonstrated, in 1978, that warfarin inhibits the enzyme vitamin K epoxide reductase, and hence interferes with vitamin K metabolism.[86]
Occupational safety
Warfarin used for pest control is a hazardous substance harmful to health. People can be exposed to warfarin in the workplace by breathing it in, swallowing it, skin absorption, and eye contact. The
It is classified as an
Society and culture
The name "warfarin" is derived from the acronym for "Wisconsin Alumni Research Foundation", plus "-arin", indicating its link with coumarin. Warfarin is a derivative of dicoumarol, an anticoagulant originally discovered in spoiled sweet clover. Dicoumarol, in turn, is from coumarin, a sweet-smelling but coagulation-inactive chemical found in "sweet" clover and tonka beans (also known as cumaru from which coumarin's name derives).
Brand names
Warfarin as a drug is marketed under many brand and generic names, including Aldocumar, Anasmol, Anticoag, Befarin, Cavamed, Cicoxil, Circuvit, Cofarin, Coumadin, Coumadine, Cumar, Farin, Foley, Haemofarin, Jantoven, Kovar, Lawarin, Maforan, Marevan, Marfarin, Marivanil, Martefarin, Morfarin, Orfarin, Panwarfin, Scheme, Simarc, Varfarin, Varfarins, Varfine, Waran, Warcok, Warf, Warfareks, Warfarin, Warfarina, Warfarine, Warfarinum, Warfen, Warfin, Warik, Warin, Warlin, and Zyfarin.[1]
Veterinary use
Warfarin is used as a poison for rats and other pests.[15][107]
Pest control
Warfarin was introduced as a poison for pest control, only later finding medical uses; in both cases it was used as an anticoagulant.[15] The use of warfarin itself as a rat poison is declining, because many rat populations have developed resistance to it,[108] and poisons of considerably greater potency have become available. However, as of 2023[update] warfarin continued to be considered a valuable tool for rodent control which minimised risk to other species.[109]
Rodents

Coumarins (4-hydroxycoumarin derivatives) are used as
Resistance to warfarin as a poison has developed in many rat populations due to an
Vampire bats
Warfarin is used to cull populations of
Brand names
Warfarin as a pest control poison is marketed under many brand and generic names, including Cov-R-Tox, Co-Rax, d-Con, Dethmor, Killgerm Sewercide, Mar-Fin, Rattunal, Rax, Rodex, Rodex Blox, Rosex, Sakarat, Sewarin, Solfarin, Sorex Warfarin, Tox-Hid, Warf, warfarin, and Warfarat. Warfarin is called coumafene in France, zoocoumarin in the Netherlands and Russia, and coumarin in Japan.[2][3]
References
- ^ a b c "Warfarin international brands". Drugs.com. 12 February 2023. Archived from the original on 5 April 2017.
- ^ a b "Pesticide Information Profiles: WARFARIN". EXTOXNET Extension Toxicology Network. September 1995. Archived from the original on 10 June 2023. Retrieved 18 February 2023.
- ^ a b "Rat poison product list". The Barn Owl Trust. 22 September 2021. Archived from the original on 18 February 2023. Retrieved 18 February 2023.
- ^ "Warfarin Use During Pregnancy". Drugs.com. 4 September 2019. Archived from the original on 9 February 2018. Retrieved 7 February 2020.
- FDA. Retrieved 22 October 2023.
- ^ "Coumadin- warfarin sodium tablet". DailyMed. Archived from the original on 26 December 2021. Retrieved 25 December 2021.
- S2CID 92210077.
- ^ a b c d e "PRODUCT INFORMATION COUMADIN" (PDF). TGA eBusiness Services. Aspen Pharma Pty Ltd. 19 January 2010. Archived from the original on 17 October 2015. Retrieved 11 December 2013.
- ^ a b c d e f g h i j k "Warfarin sodium". The American Society of Health-System Pharmacists. 13 October 2022. Archived from the original on 12 June 2018. Retrieved 16 February 2023.
- ^ PMID 22315269.
- ISBN 978-0-7817-5784-3. Archivedfrom the original on 18 September 2017.
- ISBN 978-0-12-407821-5.
- ^ "Warfarin". ScienceDirect. Archived from the original on 16 November 2021. Retrieved 16 November 2021.
- ISBN 978-3-527-32669-3. Archivedfrom the original on 18 September 2017.
- ^ PMID 29238065.
- PMID 29238065.
- hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- ISBN 978-0-85711-156-2.
- ^ "The Top 300 of 2021". ClinCalc. Archived from the original on 15 January 2024. Retrieved 14 January 2024.
- ^ "Warfarin - Drug Usage Statistics". ClinCalc. Archived from the original on 13 April 2020. Retrieved 14 January 2024.
- ^ "Coumadin". The American Society of Health-System Pharmacists. Archived from the original on 3 February 2011. Retrieved 3 April 2011.
- S2CID 80714002. Archived from the original on 3 November 2022. Retrieved 5 July 2023.)
{{cite journal}}: CS1 maint: DOI inactive as of March 2024 (link - ^ PMID 12742309.
- PMID 29706404.
- ^ PMID 15911722.
- S2CID 32069018.
- ^ "important information to know when you are taking : Coumadine and vitamine K" (PDF). U.S. National Institutes of Health. Archived from the original (PDF) on 20 October 2013. Retrieved 27 March 2014.
- ^ PMID 22315259.
- from the original on 1 February 2018.
- ^ "Warfarin diet: What foods should I avoid?". Mayo Foundation. Archived from the original on 24 August 2011. Retrieved 9 August 2011.
- PMID 22537823.
- PMID 15609884.
- ^ PMID 15721497. Archived from the original(PDF) on 3 March 2016.
- S2CID 1494933. Archived from the original(PDF) on 19 March 2012.
- PMID 30916798.
- S2CID 27269191.
- ^ a b Brayfield A (ed), Martindale: The Complete Drug Reference [online] London: Pharmaceutical Press [accessed on 24 April 2017]
- ^ "Coumadin" (PDF). U.S. Food and Drug Administration (FDA). October 2015. Archived (PDF) from the original on 23 June 2017. Retrieved 24 April 2017.
- ISBN 978-1-4160-2999-1.
- ^ Google Book Search.
- ^ ISBN 978-1-879284-36-4. Archivedfrom the original on 5 March 2024. Retrieved 26 August 2020.
- ^ PMID 22315276.
- ^ S2CID 37076001.
- PMID 25486915.
- (PDF) from the original on 27 January 2024. Retrieved 5 March 2024.
- PMID 23479259.
- PMID 17720522.
- PMID 21757117.
- PMID 17698822.
- PMID 10718793.
- PMID 10448778.
- S2CID 45496277.
- PMID 16432096.
- PMID 1444678.
- S2CID 28632135.
- PMID 21298649.
- ^ a b Abimbola Farinde (18 April 2019). "Warfarin Overanticoagulation". Medscape. Archived from the original on 19 August 2022. Retrieved 19 August 2022.
- S2CID 4733615.
- PMID 29258056.
- S2CID 10450603.
- PMID 11042238.
- from the original on 7 May 2016. Retrieved 22 August 2023.
- from the original on 23 August 2023. Retrieved 22 August 2023.
- PMID 17698826.
- ^ S2CID 43173080.
- PMID 2595433.
- PMID 15251480.
- PMID 3704105.
- PMID 10890797.
- ^ "Warfarin Anticoagulant Medication". Archived from the original on 1 July 2020. Retrieved 30 June 2020.
- ISBN 978-0-7615-1599-9.
- PMID 10902065.
- ^ Barnes J, Working Group on Complementary Medicine (September 2002). "Herb-medicine interactions: St John's Wort (Hypericum perforatum) Useful information for pharmacist" (PDF). London: Royal Pharmaceutical Society of Great Britain. p. 5. Archived from the original (PDF) on 24 September 2006. Retrieved 14 January 2009.
- ^ "Cranberry juice clot drug warning". BBC News. 18 September 2003. Archived from the original on 9 February 2008. Retrieved 18 May 2008.
- PMID 14684645.
- ^ S2CID 28468365.Free full text with registration at Medscape Archived 9 November 2010 at the Wayback Machine
- PMID 17322161.
- doi:10.1107/S056774087500427X. Archived from the originalon 20 October 2015.
- PMID 17691835.
- ISBN 978-3-946057-10-9.
- PMID 26655108.
- ISBN 978-0-19-997624-9. Archivedfrom the original on 30 June 2023. Retrieved 20 March 2023.
- S2CID 12305488.
- S2CID 38963632.
- ^ PMID 646989.
- S2CID 4424554.
- ^ S2CID 4424197.
- PMID 7861815.
- PMID 15900262.
- ^ PMID 15883587.
- ^ PMID 15930419.
- ^ PMID 18322281.
- PMID 15714076.
- ^ Jensen TS, Jacques LB, Ciccanti M, Long K, Eggleston L, Roche J (3 August 2009). "Decision Memo for Pharmacogenomic Testing for Warfarin Response (CAG-00400N)". Centers for Medicare and Medicaid Services. Archived from the original on 14 April 2018. Retrieved 14 April 2018.
- PMID 24935087.
- ^ a b c d Rajagopalan R (2018). "A Study in Scarlet". Distillations. 4 (1): 26–35. Archived from the original on 23 June 2019. Retrieved 27 June 2018.
- ^ ISBN 978-0-443-04990-3.
- ^ Schofield FW (1924). "Damaged sweet clover; the cause of a new disease in cattle simulating haemorrhagic septicemia and blackleg". J Am Vet Med Assoc. 64: 553–6.
- .
- .
- ^ "Warfarin, Molecule of the Month for February 2011, by John Maher". www.chm.bris.ac.uk. Archived from the original on 27 September 2023. Retrieved 20 December 2023.
- ^ PMID 13619027.
- ISBN 978-0-06-019524-3.
- ^ "CDC – NIOSH Pocket Guide to Chemical Hazards – Warfarin". www.cdc.gov. Archived from the original on 8 December 2015. Retrieved 27 November 2015.
- ^ "40 C.F.R.: Appendix A to Part 355—The List of Extremely Hazardous Substances and Their Threshold Planning Quantities" (21 August 2023 ed.). Government Printing Office. Archived from the original on 9 January 2023. Retrieved 22 August 2023.
- ^ ISBN 978-0-478-22035-3. Archived(PDF) from the original on 17 October 2008.
- ^ CropLife. pp. 1–29. Archived(PDF) from the original on 4 November 2021. Retrieved 23 October 2021.
- ^ "Warfarin - A valuable tool for successful rodent control whilst minimising risk to non-target species". National Pest Technicians Association. 21 October 2019. Archived from the original on 17 February 2023. Retrieved 18 February 2023.
- ^ United States Occupational Safety and Health Administration (OSHA) (16 August 1996). "Documentation for Immediately Dangerous To Life or Health Concentrations (IDLHs): Warfarin". Centers for Disease Control and Prevention. Archived from the original on 26 July 2008. Retrieved 7 July 2008.
- from the original on 26 April 2015. Retrieved 5 April 2015.
- ^ PMID 24784570.
- PMID 22696521.
Further reading
- Dean L (2012). "Warfarin Therapy and VKORC1 and CYP Genotype". In Pratt VM, McLeod HL, Rubinstein WS, Scott SA, Dean LC, Kattman BL, et al. (eds.). Medical Genetics Summaries. PMID 28520347. Bookshelf ID: NBK84174.
External links
- Warfarin in the Pesticide Properties DataBase (PPDB)
