Catecholamine

A catecholamine (
Catechol can be either a free molecule or a substituent of a larger molecule, where it represents a 1,2-dihydroxybenzene group.
Catecholamines are derived from the amino acid tyrosine, which is derived from dietary sources as well as synthesis from phenylalanine.[2] Catecholamines are water-soluble and are 50% bound to plasma proteins in circulation.
Included among catecholamines are
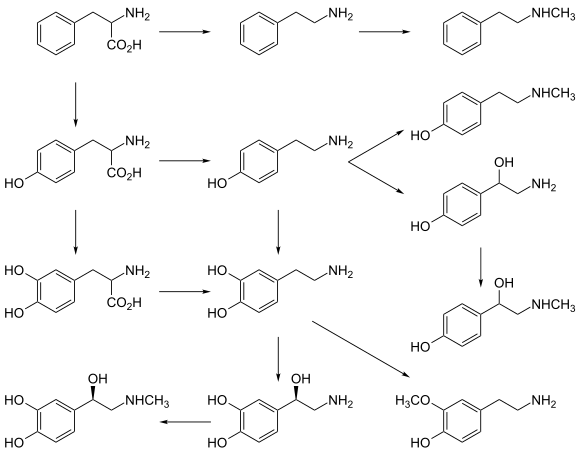
Tyrosine is created from phenylalanine by hydroxylation by the enzyme phenylalanine hydroxylase. Tyrosine is also ingested directly from dietary protein. Catecholamine-secreting cells use several reactions to convert tyrosine serially to L-DOPA and then to dopamine. Depending on the cell type, dopamine may be further converted to norepinephrine or even further converted to epinephrine.[4]
Various stimulant drugs (such as a number of substituted amphetamines) are catecholamine analogues.
Structure
Catecholamines have the distinct structure of a
Production and degradation
L-ascorbic acid as cofactors. Norepinephrine is converted into epinephrine by the enzyme phenylethanolamine N-methyltransferase (PNMT) with S-adenosyl-L-methionine as the cofactor. |
Location
Catecholamines are produced mainly by the
Biosynthesis
Dopamine is the first catecholamine synthesized from DOPA. In turn, norepinephrine and epinephrine are derived from further metabolic modification of dopamine. The enzyme dopamine hydroxylase requires copper as a cofactor (not shown in the diagram) and DOPA decarboxylase requires PLP (not shown in the diagram). The rate limiting step in catecholamine biosynthesis through the predominant metabolic pathway is the hydroxylation of L-tyrosine to L-DOPA.[9]
Catecholamine synthesis is inhibited by alpha-methyl-p-tyrosine (
The amino acids
Degradation
Catecholamines have a half-life of a few minutes when circulating in the blood. They can be degraded either by methylation by
Function
Modality
Two catecholamines,
High catecholamine levels in blood are associated with
Extremely high levels of catecholamines (also known as catecholamine toxicity) can occur in central nervous system trauma due to stimulation or damage of nuclei in the brainstem, in particular, those nuclei affecting the sympathetic nervous system. In emergency medicine, this occurrence is widely known as a "catecholamine dump".
Extremely high levels of catecholamine can also be caused by neuroendocrine tumors in the adrenal medulla, a treatable condition known as pheochromocytoma.
High levels of catecholamines can also be caused by monoamine oxidase A (MAO-A) deficiency, known as Brunner syndrome. As MAO-A is one of the enzymes responsible for degradation of these neurotransmitters, its deficiency increases the bioavailability of these neurotransmitters considerably. It occurs in the absence of pheochromocytoma, neuroendocrine tumors, and carcinoid syndrome, but it looks similar to carcinoid syndrome with symptoms such as facial flushing and aggression.[12][13]
Acute porphyria can cause elevated catecholamines.[14]
Effects
Catecholamines cause general physiological changes that prepare the body for physical activity (the
Catecholamine is secreted into urine after being broken down, and its secretion level can be measured for the diagnosis of illnesses associated with catecholamine levels in the body.
Function in plants
This section contains too many or overly lengthy quotations. (December 2024) |
They have been found in 44 plant families, but no essential metabolic function has been established for them. They are precursors of benzo[c]phenanthridine
embryogenesis from in vitro cultures, and flowering. CAs inhibit indole-3-acetic acid oxidation and enhance ethylene biosynthesis. They have also been shown to enhance synergistically various effects of gibberellins.[17]
Testing for catecholamines
Catecholamines are secreted by cells in tissues of different systems of the human body, mostly by the nervous and the endocrine systems. The adrenal glands secrete certain catecholamines into the blood when the person is physically or mentally stressed and this is usually a healthy physiological response.[citation needed] However, acute or chronic excess of circulating catecholamines can potentially increase blood pressure and heart rate to very high levels and eventually provoke dangerous effects. Tests for fractionated plasma free metanephrines or the urine metanephrines are used to confirm or exclude certain diseases when the doctor identifies signs of hypertension and tachycardia that don't adequately respond to treatment.[18][19] Each of the tests measure the amount of adrenaline and noradrenaline metabolites, respectively called metanephrine and normetanephrine.
Blood tests are also done to analyze the amount of catecholamines present in the body.
Catecholamine tests are done to identify rare tumors at the adrenal gland or in the nervous system. Catecholamine tests provide information relative to tumors such as: pheochromocytoma, paraganglioma, and neuroblastoma.[20][21]
See also
References
- ^ Fitzgerald, P. A. (2011). "Chapter 11. Adrenal Medulla and Paraganglia". In Gardner, D. G.; Shoback, D. (eds.). Greenspan's Basic & Clinical Endocrinology (9th ed.). New York: McGraw-Hill. Retrieved October 26, 2011.
- ISBN 978-0-87893-697-7.
- ^ "Catecholamines". Health Library. San Diego, CA: University of California. Archived from the original on July 16, 2011.
- S2CID 86229251.
- PMID 19948186.
- PMID 15860375.
- PMID 24374199.
- ^ S2CID 2578817.
- .
- S2CID 12825309.
- PMID 31082164, retrieved 2024-06-28
- PMID 12140786.
- PMID 8862875.
- PMID 17660335.
- ISBN 978-0-17-035484-4.
- ^ "Catecholamines in Urine". webmd.com. Retrieved 4 May 2017.
- S2CID 41493767.
- ^ "Plasma Free Metanephrines | Lab Tests Online". labtestsonline.org. Retrieved 2019-12-24.
- ^ "Urine Metanephrines | Lab Tests Online". labtestsonline.org. 6 December 2019. Retrieved 2019-12-24.
- ^ "Catecholamine Urine & Blood Tests". WebMD. Retrieved 2019-10-09.
- ^ "Catecholamines". labtestsonline.org. Retrieved 2019-10-09.
External links
- Catecholamines at the U.S. National Library of Medicine Medical Subject Headings (MeSH)