User talk:Wiki CRUK John/Pancreatic cancer (version g)
| Wiki CRUK John/Pancreatic cancer (version g) | |
|---|---|
| Specialty | Oncology |
Pancreatic cancer arises when
Signs and symptoms of the most common form of pancreatic cancer may include yellow skin, abdominal or back pain, unexplained weight loss, light-colored stools, dark urine and loss of appetite. There are usually no symptoms in the disease's early stages, and symptoms that are specific enough to suspect pancreatic cancer typically do not develop until the disease has reached an advanced stage.[2] By the time of diagnosis, pancreatic cancer has often spread to other parts of the body.[3][4]
Pancreatic cancer rarely occurs before the age of 40, and more than half of cases of pancreatic adenocarcinoma occur in those over 70.
The risk of developing pancreatic cancer is lower among non-smokers, and people who maintain a healthy weight and limit their consumption of red or processed meat.[8] A smoker's chance of developing the disease decreases if they stop smoking, and almost returns to that of the rest of the population after 20 years.[4] Pancreatic cancer can be treated with surgery, radiotherapy, chemotherapy, palliative care, or a combination of these. Treatment options are partly based on the cancer stage. Surgery is the only treatment that can cure the disease; it may also be done to try to improve quality of life without the potential for cure.[9] Pain management and medications to improve digestion are sometimes needed.[3] Early palliative care is recommended even for those receiving treatment that aims for a cure.[10][11]
In 2012, pancreatic cancers of all types were the seventh most common cause of cancer deaths, resulting in 330,000 deaths globally.[4] In the United States, pancreatic cancer is the fourth most common cause of deaths due to cancer.[12][13] The disease occurs most often in the developed world, where about 70% of the new cases in 2012 originated.[4] Pancreatic adenocarcinoma typically has a very poor prognosis: after diagnosis, 25% of people survive one year and 5% live for five years.[4][14] For cancers diagnosed early, the five-year survival rate rises to about 20%.[15] Neuroendocrine cancers have better outcomes; at five years from diagnosis, 65% of those diagnosed are living, though survival varies considerably depending on the type of tumor.[4]
Types
The many types of pancreatic cancer can be divided into two general groups. The vast majority of cases (about 99%) occur in the part of the pancreas which produces
Exocrine cancers
The exocrine group is dominated by pancreatic adenocarcinoma (variations of this name may add "invasive" and "ductal"), which is by far the most common type, representing about 85% of all pancreatic cancers.[2] This is despite the fact that the tissue from which it arises - the pancreatic ductal epithelium - represents less than 10% of the pancreas by cell volume.[18] This cancer originates in the ducts that carry certain hormones and enzymes away from the pancreas. About 60–70% of adenocarcinomas occur in the 'head' of the pancreas (see diagram, right).[2]
The next most common type, acinar cell carcinoma of the pancreas, arises in the clusters of cells that produce these enzymes, and represents 5% of exocrine pancreas cancers. Like the 'functioning' endocrine cancers described below, acinar cell carcinomas may cause over-production of certain molecules, in this case digestive enzymes, which may cause symptoms such as skin rashes and joint pain.
Cystadenocarcinomas account for 1% of pancreatic cancers, and they have a better prognosis than the other exocrine types.[19]
Pancreatic mucinous cystic neoplasms are a broad group of pancreas tumors that have varying malignant potential. They are being detected at a greatly increased rate as CT scans become more powerful and common, and discussion continues as how best to assess and treat them, given that many are benign.[21]
Neuroendocrine
The small minority of tumors that arise elsewhere in the pancreas are mainly pancreatic
As with other neuroendocrine tumors, the history of the terminology and classification of PanNETs is complex.
Signs and symptoms

Since pancreatic cancer usually does not cause recognizable symptoms in its early stages, the disease is typically not diagnosed until it has spread beyond the pancreas itself.[6] This is one of the main reasons for the generally poor survival rates. Exceptions to this are the functioning PanNETs, where over-production of various active hormones can give rise to symptoms (which depend on the type of hormone).[25]
Bearing in mind that the disease is rarely diagnosed before the age of 40, common symptoms of pancreatic adenocarcinoma occurring before diagnosis include:
- Pain in the upper abdomen or back, often spreading from around the stomach to the back. The location of the pain can indicate the part of the pancreas where a tumor is located. The pain may be worse at night and may increase over time to become severe and unremitting. It may be slightly relieved by bending forward.[19] In the UK, about half of new cases of pancreatic cancer are diagnosed following a visit to a hospital emergency department for pain or jaundice. In up to two-thirds of people abdominal pain is the main symptom, for 46% of the total accompanied by jaundice, with 13% having jaundice without pain.[3]
- Jaundice, a yellow tint to the whites of the eyes or skin, with or without pain, and possibly in combination with darkened urine. This results when a cancer in the head of the pancreas obstructs the common bile duct as it runs through the pancreas.[26]
- poor digestion.[3]
- The tumor may compress neighboring organs, disrupting digestive processes and making it difficult for the stomach to empty, which may cause nausea and a feeling of fullness. The undigested fat leads to foul-smelling, fatty feces that are difficult to flush away.[3] Constipation is common.[27]
- At least 50% of people with pancreatic adenocarcinoma have diabetes at the time of diagnosis.[2] While long-standing diabetes is a known risk factor for pancreatic cancer (see Risk factors), the cancer can itself cause diabetes, in which case recent onset of diabetes could be considered an early sign of the disease.[28] People over 50 who develop diabetes have eight times the usual risk of developing pancreatic adenocarcinoma within three years, after which the relative risk declines.[3]
Other findings
- Trousseau's syndrome, in which blood clots form spontaneously in the portal blood vessels, the deep veins of the extremities, or the superficial veins anywhere on the body, may be associated with pancreatic cancer, and is found in about 10% of cases.[5]
- Clinical depression has been reported in association with pancreatic cancer in some 10–20% of cases, and can be a hindrance to optimal management. The depression sometimes appears before the diagnosis of cancer, suggesting that it may be brought on by the biology of the disease.[5]
Other common manifestations of the disease include: weakness and tiring easily; dry mouth; sleep problems; and a palpable abdominal mass."[27]
Symptoms of spread (metastasis)

The spread of pancreatic cancer to other organs (
Cancers in the pancreas may also be
Risk factors
Risk factors for pancreatic adenocarcinoma include:[2][3][4][31]
- Age, gender, and race; the risk of developing pancreatic cancer increases with age. Most cases occur after age 65,African Americans, though incidence in Africa is low.[4]
- Cigarette smoking is the best-established avoidable risk factor for pancreatic cancer, approximately doubling risk among long-term smokers, the risk increasing with the number of cigarettes smoked and the years of smoking. The risk declines slowly after smoking cessation, taking some 20 years to return to almost that of non-smokers.[32]
- Obesity; a BMI greater than 35 increases relative risk by about half.[3]
- Family history; 5–10% of pancreatic cancer cases have an inherited component, where people have a family history of pancreatic cancer.
- Pancreatic cancer has been associated with the following other rare hereditary syndromes:
- Chronic pancreatitis appears to almost triple risk, and as with diabetes, new-onset pancreatitis may be a symptom of a tumor.[5] The risk of pancreatic cancer in individuals with familial pancreatitis is particularly high.[5][33]
- Diabetes mellitus is a risk factor for pancreatic cancer and (as noted in the Signs and symptoms section) new-onset diabetes may also be an early sign of the disease. People who have been diagnosed with Type 2 diabetes for longer than ten years may have a 50% increased risk, as compared with non-diabetics.[5]
- Specific types of food (as distinct from obesity) have not been clearly shown to increase the risk of pancreatic cancer.[2] Dietary factors for which there is some evidence of slightly increased risk include processed meat, red meat, and meat cooked at very high temperatures (e.g. by frying, broiling or barbecuing).[35][36]
Alcohol
Drinking alcohol excessively is a major cause of chronic pancreatitis, which in turn predisposes to pancreatic cancer. However, considerable research has failed to firmly establish alcohol consumption as a direct risk factor for pancreatic cancer. Overall, the association is consistently weak and the majority of studies have found no association, with smoking a strong confounding factor. The evidence is stronger for a link with heavy drinking, of at least six drinks per day.[5][37]
Diagnosis
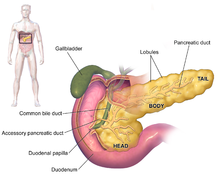

The symptoms of pancreatic adenocarcinoma do not usually appear in the disease's early stages, and are individually not distinctive to the disease.[3][5][26] The symptoms at diagnosis vary according to the location of the cancer in the pancreas, which anatomists divide (from left to right on most diagrams) into the thick head, the neck, and the tapering body, ending in the tail.
Regardless of a tumour's location, the most common symptom is unexplained weight loss, which may be considerable. A large minority (between 35% and 47%) of people diagnosed with the disease will have had nausea, vomiting or a feeling of weakness.
Tumors in the head of the pancreas typically also cause jaundice, pain, loss of appetite, dark urine, and light-colored stools. Tumors in the body and tail typically also cause pain.[26]
People sometimes have recent onset of atypical type 2 diabetes that is difficult to control, a history of recent but unexplained blood vessel inflammation caused by blood clots (thrombophlebitis) known as Trousseau sign, or a previous attack of pancreatitis.[26] A doctor may suspect pancreatic cancer when the onset of diabetes in someone over 50-years-old is accompanied by typical symptoms such as unexplained weight loss, persistent abdominal or back pain, indigestion, vomiting, or fatty feces.[3] Jaundice accompanied by a painlessly swollen gallbladder (known as Courvoisier's sign) may also raise suspicion, and can help differentiate pancreatic cancer from gallstones.[38]
A biopsy by
The most common form of pancreatic cancer (adenocarcinoma) is typically characterized by moderately to
Staging
Exocrine cancers
Pancreatic cancer is usually staged following a CT scan.[26] The most widely used cancer staging system for pancreatic cancer is the one formulated by the American Joint Committee on Cancer (AJCC) together with the Union for International Cancer Control (UICC). The AJCC-UICC staging system designates four main overall stages, ranging from early to advanced disease, based on TNM classification of Tumor size, spread to lymph Nodes, and Metastasis.[40]
To help decide treatment, the tumors are also divided into three broader categories based on whether surgical removal seems possible: in this way, tumors are judged to be "resectable", "borderline resectable", or "unresectable".
- Pancreatic cancer staging (TNM classification)
-
Stage T1 pancreatic cancer
-
Stage T2 pancreatic cancer
-
Stage T3 pancreatic cancer
-
Stage T4 pancreatic cancer
-
Pancreatic cancer in nearby lymph nodes – Stage N1

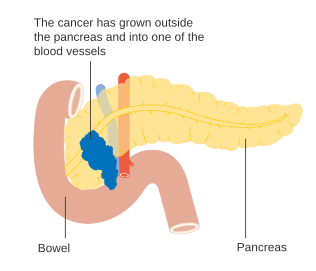
Locally advanced adenocarcinomas have spread into neighboring organs, which may be any of the following (in roughly decreasing order of frequency): the duodenum, stomach, transverse colon, spleen, adrenal gland, or kidney. Very often they also spread to the important blood or lymphatic vessels and nerves that run close to the pancreas, making surgery far more difficult. Typical sites for metastasic spread (stage IV disease) are the liver, peritoneal cavity and lungs, all of which occur in 50% or more of fully advanced cases.[42]
PanNETs
The 2010 WHO classification of tumors of the digestive system grades all the neuroendocrine tumors into three categories, based on their degree of cellular differentiation (from "NET G1" through to the poorly-differentiated "NET G3").[17] The U.S. National Comprehensive Cancer Network recommends use of the same AJCC-UICC staging system as pancreatic adenocarcinoma.[43]: 52 Using this scheme, the stage-by-stage outcomes for PanNETs are dissimilar to those of the exocrine cancers.[44] A different TNM system for PanNETs has been proposed by the European Neuroendocrine Tumor Society.[17]
Precursors

Exocrine cancers

These cancers are thought to arise from several types of
The first is pancreatic
Secondly, intraductal papillary mucinous neoplasms (IPMNs) are macroscopic lesions, which occur in about 2% of all adults, rising to about 10% by age 70, and have about a 25% risk of developing into invasive cancer. They also very often have KRAS gene mutations, in about 40–65% of cases, and in the GNAS Gs alpha subunit and RNF43, affecting the Wnt signaling pathway.[2] Even if removed surgically, there remains a considerably increased risk of pancreatic cancer developing subsequently.[5]
The last type, pancreatic mucinous cystic neoplasms (MCNs) mainly occur in women, and may remain benign or progress to cancer.[45] If they become large, cause symptoms, or have suspicious features, they can usually be successfully removed by surgery.[5]
The genetic events found in ductal adenocarcinoma have been well characterized, and complete
PanNETs
The genes often found mutated in PanNETs are different from those in pancreatic adenocarcinoma.
Prevention and screening
Apart from not smoking, the
In the general population, screening of large groups is not currently considered effective, although newer techniques, and the screening of tightly targeted groups, are being evaluated.[49][50] Nevertheless, regular screening with endoscopic ultrasound and MRI/CT imaging is recommended for those at high risk from inherited genetics.[6][39][50][51]
Management
Exocrine cancer
A key assessment that is made after diagnosis is whether surgical removal of the tumor is possible (see Staging), as this is the only cure for this cancer. Whether or not surgical resection can be offered depends on how much the cancer has spread. The exact location of the tumor is also a significant factor, and CT can show how it relates to the major blood vessels passing close to the pancreas. The general health of the person must also be assessed, though age in itself is not an obstacle to surgery.[5]
Chemotherapy and, to a lesser extent, radiotherapy are likely to be offered to most people, whether or not surgery is possible. Specialists advise that the management of pancreatic cancer should be in the hands of a
Surgery

Surgery with the intention of a cure is only possible in around one-fifth (20%) of new cases.[3] Although CT scans help, in practice it can be difficult to determine whether the tumor can be fully removed (its "resectability"), and it may only become apparent during surgery that it is not possible to successfully remove the tumor without damaging other vital tissues. Whether or not surgical resection can be offered depends on various factors, including the precise extent of local anatomical adjacency to, or involvement of, the venous or arterial blood vessels,[2] as well as surgical expertise and a careful consideration of projected post-operative recovery.[52][53] The age of the person is not in itself a reason not to operate, but their general performance status needs to be adequate for a major operation.[3]
One particular feature that is looked is the encouraging presence, or discouraging absence, of a clear layer or plane of fat giving a barrier between the tumor and the vessels.[5] Traditionally, an assessment is made of the tumor's proximity to major venous or arterial vessels, in terms of "abutment" (defined as the tumor touching no more than half a blood vessel's circumference without any fat to separate it), "encasement" (when the tumor encloses most of the vessel's circumference), or full vessel involvement.[54]: 22 A resection that includes encased sections of blood vessels may be possible in some cases,[55][56] particularly if preliminary neoadjuvant therapy is feasible,[57][58][59] using chemotherapy[53][54]: 36 [60] and/or radiotherapy.[54]: 29–30
Even when the operation appears to have been successful, cancerous cells are often found around the edges ("

For cancers involving the head of the pancreas, the
Although curative surgery no longer entails the very high death rates that occurred until the 1980s, a high proportion of people (about 30–45%) still have to be treated for post-operative sickness that is not caused by the cancer itself. The most common complication of surgery is difficulty in emptying the stomach.[5] Certain more limited surgical procedures may also be used to ease symptoms (see Palliative care). For instance, if the cancer is invading or compressing the duodenum or colon. In such cases, bypass surgery might overcome the obstruction and improve quality of life but is not intended as a cure.[3]
Chemotherapy
After surgery,
The FOLFIRINOX chemotherapy regimen using four drugs was found more effective than gemcitabine, but with substantial side effects, and is thus only suitable for people with good performance status. This is also true of protein-bound paclitaxel (nab-paclitaxel), which was licensed by the FDA in 2013 for use with gemcitabine in pancreas cancer.[68] By the end of 2013, both FOLFIRINOX and nab-paclitaxel with gemcitabine were regarded as good choices for those able to tolerate the side-effects, and gemcitabine remained an effective option for those who were not. A head-to-head trial between the two new options is awaited, and trials investigating other variations continue. However, the changes of the last few years have only increased survival times by a few months.[65] Clinical trials are often conducted for novel adjuvant therapies.[6]
Radiotherapy
The role of radiotherapy as an auxiliary (adjuvant) treatment after potentially curative surgery has been controversial since the 1980s.[5] The European Society for Medical Oncology recommends that adjuvant radiotherapy should only be used for people enrolled in clinical trials.[39] However, there is a continuing tendency for clinicians in the US to be more ready to use adjuvant radiotherapy than those in Europe. Many clinical trials have tested a variety of treatment combinations since the 1980s, but have failed to settle the matter conclusively.[5][6]
Radiotherapy may form part of treatment to attempt to shrink a tumor to a resectable state, but its use on unresectable tumors remains controversial as there are conflicting results from clinical trials. The preliminary results of one trial, presented in 2013, "markedly reduced enthusiasm" for its use on locally advanced tumors.[2]
PanNETs
Treatment of PanNETs, including the less common
For localized tumors, the surgical procedure may be much less extensive than the types of surgery used to treat pancreatic adenocarcinoma described above, but otherwise surgical procedures are similar to those for exocrine tumors. The range of possible outcomes varies greatly; some types have a very high survival rate after surgery while others have a poor outlook. As all this group are rare, guidelines emphasize that treatment should be undertaken in a specialized center.[23][17]Use of liver transplantation may be considered in certain cases of liver metastasis.[72]
For functioning tumors, the
Radiation therapy is occasionally used if there is pain due to anatomic extension, such as
Palliative care
Palliative care is medical care which focuses on treatment of symptoms from serious illness, such as cancer, and improving quality of life.[84] Because pancreatic adenocarcinoma is usually diagnosed after it has progressed to an advanced stage, palliative care as a treatment of symptoms is often the only treatment possible.[85]
Palliative care focuses not on treating the underlying cancer, but on treating symptoms such as
Other symptoms or complications that can be treated with palliative surgery are obstruction by the tumor of the intestines or bile ducts. For the latter, which occurs in well over half of cases, a small metal tube called a stent may be inserted by endoscope to keep the ducts draining.[26] Palliative care can also help treat depression that often comes with diagnosis of pancreatic cancer.[5]
Both surgery and advanced inoperable tumors often lead to
Outcomes
| Clinical stage | Five-year survival (%) – U.S., diagnoses 1992–98 | |
|---|---|---|
| Exocrine pancreatic cancer | Neuroendocrine treated with surgery | |
| IA / I | 14 | 61 |
| IB | 12 | |
| IIA / II | 7 | 52 |
| IIB | 5 | |
| III | 3 | 41 |
| IV | 1 | 16 |
Pancreatic adenocarcinoma and the other less common exocrine cancers have a very poor prognosis, as they are normally diagnosed at a late stage when the cancer is already locally advanced or has spread to other parts of the body.[2] Outcomes are much better for PanNETs: many are benign and completely without clinical symptoms, and even those cases not treatable with surgery have an average five-year survival rate of 16%,[41] although the outlook varies considerably varies according to the type.[25]
For locally advanced and
Distribution

As of 2012, pancreatic cancer resulted in 330,000 deaths globally,[4] up from 310,000 in 2010 and 200,000 in 1990.[90] In 2014, an estimated 46,000 people in the US are expected to be diagnosed with pancreatic cancer and 40,000 to die of it.[2] Although it accounts for only 2.5% of new cases, pancreatic cancer is responsible for 6% of cancer deaths each year.[91] It is the seventh highest cause of death from cancer worldwide.[4]
Globally pancreatic cancer is the 11th most common cancer in women and the 12th most common in men.
Pancreatic cancer is the 10th most common cancer in the UK (around 8,800 people were diagnosed with the disease in 2011), and it is the 5th most common cause of cancer death (around 8,700 people died in 2012).[94]
PanNETs
The annual
History
The earliest recognition of pancreatic cancer has been attributed to the 18th-century Italian scientist
Regarding the recognition of PanNETs, the possibility of cancer of the islet cells was initially suggested in 1888. The first case of
The first reported partial pancreaticoduodenectomy was performed by the Italian surgeon Alessandro Codivilla in 1898, but the patient only survived 18 days before succumbing to complications. Early operations were compromised partly because of mistaken beliefs that people would die if their duodenum was removed, and also, at first, if the flow of pancreatic juices stopped. Later it was thought, also mistakenly, that the pancreatic duct could simply be tied up without serious adverse effects; in fact it will very often leak later on. In 1907-08, after some more unsuccessful operations by other surgeons, experimental procedures were tried on corpses by French surgeons.[96]
In 1912 the German surgeon
The discovery in the late 1930s that vitamin K prevented bleeding with jaundice, and the development of blood transfusion as an everyday process, both improved post-operative survival,[96] but about 25% of people never left hospital alive as late as the 1970s.[97] In the 1970s a group of American surgeons wrote urging that the procedure was too dangerous and should be abandoned. Since then outcomes in larger centers have improved considerably, and mortality from the operation is often less than 4%.[18] In 2006 a report was published of a series of 1,000 consecutive pancreaticoduodenectomies performed by a single surgeon from Johns Hopkins Hospital between 1969 and 2003. The rate of these operations had increased steadily over this period, with only three of them before 1980, and the median operating time reduced from 8.8 hours in the 1970s to 5.5 hours in the 2000s, and mortality within 30 days or in hospital was only 1%.[96][97] Another series of 2,050 operations at the Massachusetts General Hospital between 1941 and 2011 showed a similar picture of improvement.[98]
Small precancerous neoplasms for many pancreatic cancers are being detected at greatly increased rates by modern medical imaging. One type, the intraductal papillary mucinous neoplasm (IPMN) was first described by Japanese researchers in 1982; "For the next decade, little attention was paid to this report; however, over the subsequent 15 years, there has been a virtual explosion in the recognition of this tumor."[42]
Research directions
Worldwide efforts on many levels are underway to understand pancreatic cancer, but progress has been slow, particularly into understanding the disease's causes.[99] There are several fundamental unanswered questions.[100][101] The nature of the changes that lead to the disease are being intensely investigated, such as the roles played by genes such as KRAS and p53.[33][102][103] A key question is the timing of events as the disease develops and progresses – particularly the role of diabetes,[104] and how and when the disease spreads.[105]
Research on early detection is ongoing.
Another area of interest is in assessing whether keyhole surgery (
Efforts are underway to develop new drugs.
See also
- Gastrointestinal cancer
- Pancreatic Cancer Action (organization in the UK)
- Lustgarten Foundation for Pancreatic Cancer Research (organization in the US)
References
- ^ "What is Cancer? Defining Cancer". National Cancer Institute. National Institutes of Health. 7 March 2014. Retrieved 5 December 2014.
- ^ PMID 25207767.
- ^ PMID 22592847.
- ^ ISBN 92-832-0429-8.
- ^ PMID 23856911.
- ^ PMID 21620466.
- PMID 20208319.
- ^ "Can pancreatic cancer be prevented?". American Cancer Society. 11 June 2014. Retrieved 13 November 2014.
- ^ "Pancreatic Cancer Treatment (PDQ®) Patient Version". National Cancer Institute. National Institutes of Health. 17 April 2014. Retrieved 8 June 2014.
- PMID 23846935.
- PMID 24182608.
- PMID 18695761.
- ^ "Lifetime Risk of Developing or Dying From Cancer". American Cancer Society. 1 October 2014. Retrieved 1 December 2014. The top three vary by gender, and include breast cancer for women and prostate cancer for men.
- ^ "Cancer Facts & Figures 2010" (PDF). American Cancer Society. 2010. Retrieved 5 December 2014. See p. 4 for incidence estimates, and p. 19 for survival percentages.
- ^ a b "Pancreatic Cancer Treatment (PDQ®) Health Professional Version". National Cancer Institute. National Institutes of Health. 21 February 2014. Retrieved 24 November 2014. "The highest cure rate occurs if the tumor is truly localized to the pancreas; however, this stage of disease accounts for less than 20% of cases. In cases with localized disease and small cancers (<2 cm) with no lymph node metastases and no extension beyond the capsule of the pancreas, complete surgical resection is associated with an actuarial five-year survival rate of 18% to 24%."
- ISBN 978-0-7637-8047-0.
- ^ ).
- ^ ISBN 978-1-4511-0545-2. Online edition, with updates to 2014
- ^ ISBN 978-1-1187-1325-9.
- ^ a b c "Types of Pancreas Tumors". The Sol Goldman Pancreas Cancer Research Center. Johns Hopkins Medicine. 2012. Retrieved 18 November 2014.
- PMID 23622140.
- ^ PMID 20664470.
- ^ PMID 22198808.
- ^ The Medical Subject Headings indexing system refers to "islet cell carcinoma", which is subdivided into gastrinoma, glucagonoma, somatostatinoma and VIPoma. See: 2014 MeSH tree at "Pancreatic Neoplasms [C04.588.322.475]" 16 October 2014
- ^ a b "Islet Cell Tumors of the Pancreas / Endocrine Neoplasms of the Pancreas". The Sol Goldman Pancreas Cancer Research Center. Johns Hopkins Medicine. 2012. Retrieved 5 January 2015.
- ^ PMID 24784121.
- ^ ISBN 9780781768849.
- PMID 19111249.
- ^ "Chapter 15; Pancreas". Manual for Staging of Cancer (PDF) (2nd ed.). American Joint Committee on Cancer. pp. 95–8. See page 95 for citation regarding "... lesser degree of involvement of bones and brain and other anatomical sites."
- PMID 25320654.
- ^ "Causes of pancreatic cancer". NHS Choices. National Health Service, England. 7 October 2014. Retrieved 5 December 2014.
- PMID 22104574.
- ^ PMID 24624093.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - PMID 19349734.
- ^ "Cancer Facts and Figures 2014" (PDF). American Cancer Society. Retrieved 5 January 2015., p. 19, "Though evidence is still accumulating, consumption of red or processed meat, or meat cooked at very high temperatures, may slightly increase risk."
- PMID 22240790.
- ^ PMID 24403441.
- PMID 19190960.
- ^ PMID 22997452.
- PMID 20555103.
- ^ a b c "Staging of pancreatic cancer". American Cancer Society. 11 June 2014. Retrieved 29 September 2014.
- ^ ISBN 978-0-7817-6546-6. Retrieved 3 November 2014.
- ^ a b c d "Neuroendocrine tumors, NCCN Guidelines Version 1.2015" (PDF). NCCN Guidelines. National Comprehensive Cancer Network, Inc. 11 November 2014. Retrieved 25 December 2014.
- ^ National Cancer Institute. Pancreatic Neuroendocrine Tumors (Islet Cell Tumors) Treatment (PDQ®) Incidence and Mortality [2]
- PMID 21886451.
- ^ PMID 24310147.
- PMID 22723327.
- ^ "Diet and activity factors that affect risks for certain cancers: Pancreatic cancer section". American Cancer Society. 20 August 2012. Retrieved 4 November 2014.
- ^ PMID 25170208.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - ^ PMID 25170207.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - PMID 21633635.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - PMID 24578248.
- ^ PMID 22064622.
- ^ a b c "Pancreatic adenocarcinoma. NCCN Guidelines Version 1.2015" (PDF). NCCN Guidelines. National Comprehensive Cancer Network, Inc. 4 December 2014. Retrieved 26 December 2014.
- PMID 25339810.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - PMID 25152577.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - PMID 25071332.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - PMID 20422030.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - PMID 25519932.
- PMID 25089113.
- PMID 25499079.
- ^ PMID 25152582.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - PMID 24272022.
- PMID 23852311.
- ^ PMID 24683721.
- Wolters Kluwer Health. Retrieved 18 November 2014.
- ^ "Cancer Drug Information: FDA Approval for Erlotinib Hydrochloride". National Cancer Institute. National Institutes of Health. 3 July 2013. Retrieved 5 December 2014.
- PMID 24882381.
- PMID 22261872.
- PMID 22261919.
- PMID 22262022.
- PMID 25332984.
- ^ Nick Mulcahy (17 December 2014). "FDA Approves Lanreotide for Neuroendocrine Tumors". Medscape Medical News. WebMD LLC. Retrieved 25 December 2014.
- ^ Everolimus Approved for Pancreatic Neuroendocrine Tumors. The ASCO Post. May 15, 2011, Volume 2, Issue 8 http://ascopost.com/articles/may-15-2011/everolimus-approved-for-pancreatic-neuroendocrine-tumors/
- ^ National Cancer Institute. Cancer Drug Information. FDA Approval for Sunitinib Malate. Pancreatic Neuroendocrine Tumors http://www.cancer.gov/cancertopics/druginfo/fda-sunitinib-malate
- PMID 24618436.
- ISBN 978-0-615-41824-7.
- PMID 22221516.
- PMID 25297671.
- PMID 20113677.
- PMID 25065935.
- PMID 25480314.
- PMID 25366583.
- ^ "Palliative or Supportive Care". American Cancer Society. 2014. Retrieved 20 August 2014.
- PMID 25132756.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - ^ "If treatment for pancreatic cancer stops working". American Cancer Society. 11 June 2014. Retrieved 20 August 2014.
- PMID 21412903.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ "Cancer Facts and Figures 2014" (PDF). American Cancer Society. Retrieved 5 January 2015., Table, p. 18, rates adjusted for normal life expectancy
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. Retrieved 11 November 2009.
- PMID 23245604.
- PMID 17237035.
- ^ "What are the key statistics about pancreatic cancer?". American Cancer Society. 11 June 2014. Retrieved 11 November 2014.
- ^ "Pancreatic cancer statistics". Cancer Research UK. Retrieved 18 December 2014.; "In 2010, in the UK, the lifetime risk of developing pancreatic cancer is 1 in 73 for men and 1 in 74 for women", noting "The lifetime risk ... has been calculated ... using the 'Current Probability' method; this is a different method used from most other cancer sites since the possibility of having more than one diagnosis of pancreatic cancer over the course of their lifetime is very low"
- ^ "Pancreatic cancer statistics". Cancer Research UK. Retrieved 28 October 2014.
- ^ PMID 6356946.
- ^ PMID 21609369.
- ^ PMID 16794383.
- PMID 22770961.
- PMID 19561317.
- ^ "What's new in pancreatic cancer research and treatment?". American Cancer Society. 11 June 2014. Retrieved 17 July 2014.
- ^ "Pancreatic cancer research". Cancer Research UK. Retrieved 17 July 2014.
- ^ "Australian Pancreatic Genome Initiative". Garvan Institute. Retrieved 17 July 2014.
- PMID 23103869.
- ^ PMID 19111249.
- PMID 25388820.
- ^ "About EUROPAC". European Registry of Hereditary Pancreatitis and Familial Pancreatic Cancer (EUROPAC). University of Liverpool. Retrieved 17 July 2014.
- PMID 25436129.
- PMID 25479908.
- .
- PMID 24331180.
- PMID 25307210.
- PMID 25078674.
- PMID 24631947.
- ^ PMID 25152585.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - ^ PMID 25337831.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - PMID 25170201.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - PMID 24379681.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - PMID 23849556.
- doi:10.2147/OV.S53858.)
{{cite journal}}: CS1 maint: unflagged free DOI (link - PMID 25341927.
External links