Seminal vesicles
| Seminal vesicle | |
|---|---|
urinary tract and male reproductive system, with the seminal vesicles seen top right | |
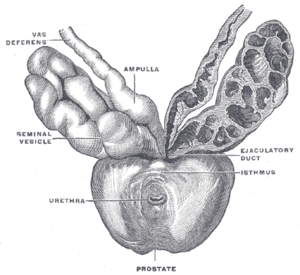 The seminal vesicles seen near the prostate, viewed from in front and above. | |
| Details | |
| Precursor | Wolffian duct |
| System | Male reproductive system |
| Artery | Inferior vesical artery, middle rectal artery |
| Lymph | External iliac lymph nodes, internal iliac lymph nodes |
| Identifiers | |
| Latin | vesiculae seminales, glandulae vesiculosae |
| MeSH | D012669 |
| TA98 | A09.3.06.001 |
| TA2 | 3631 |
| FMA | 19386 |
| Anatomical terminology] | |
The seminal vesicles (also called vesicular glands
The vesicles are 5–10 cm in size, 3–5 cm in diameter, and are located between the
Inflammation of the seminal vesicles is called seminal vesiculitis and most often is due to bacterial infection as a result of a
The seminal vesicles have been described as early as the second century AD by Galen, although the vesicles only received their name much later, as they were initially described using the term from which the word prostate is derived.
Structure
The seminal vesicles are a pair of glands in males that are positioned below the
The vesicles receive blood supply from the vesiculodeferential artery, and also from the
The vesicles lie behind the bladder at the end of the vasa deferentia. They lie in the space between the bladder and the rectum; the bladder and prostate lie in front, the tip of the ureter as it enters the bladder above, and Denonvilliers' fascia and the rectum behind.[3]
Development
In the developing
In the male, under the influence of
The development and maintenance of the seminal vesicles, as well as their secretion and size/weight, are highly dependent on
Microanatomy
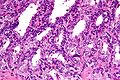
The inner lining of the seminal vesicles (the
-
Low magnification micrograph of seminal vesicle. H&E stain.
-
High magnification micrograph of seminal vesicle. H&E stain.
Function
The seminal vesicles secrete a significant proportion of the fluid that ultimately becomes
About 70-85% of the seminal fluid in humans originates from the seminal vesicles.[10] The fluid consists of nutrients including fructose and citric acid, prostaglandins, and fibrinogen.[9] Fructose is not produced anywhere else in the body except in the seminal vesicles. It provides a forensic test in rape cases.
Nutrients help support
Clinical significance
Disease
Diseases of the seminal vesicles as opposed to that of prostate gland are extremely rare and are infrequently reported in the medical literature.[11]
Seminal vesiculitis (also known as spermatocystitis) is an inflammation of the seminal vesicles, most often caused by bacterial infection.
Benign tumours of the seminal vesicles are rare.
Investigations
Symptoms due to diseases of the seminal vesicles may be vague and not able to be specifically attributable to the vesicles themselves; additionally, some conditions such as tumours or cysts may not cause any symptoms at all.[8] When diseases is suspected, such as due to pain on ejaculation, blood in the urine, infertility, due to urinary tract obstruction, further investigations may be conducted.[8]
A
A urine specimen may be collected, and is likely to demonstrate blood within the urine.[8] Laboratory examination of seminal vesicle fluid requires a semen sample, e.g. for semen culture or semen analysis. Fructose levels provide a measure of seminal vesicle function and, if absent, bilateral agenesis or obstruction is suspected.[12]
Imaging of the vesicles is provided by
Other animals
The evolution of seminal vesicles may have been influenced by sexual selection. They occur in many groups of mammals,[19] but are absent in marsupials,[20] monotremes, and carnivorans.[21][22] The function is similar in all mammals they are present in, which is to secrete a fluid as part of semen that is ejaculated during the sexual response.[19]
History
The action of the seminal vesicles has been described as early the second century AD by Galen, as "glandular bodies" that secrete substances alongside semen during reproduction.[21] By the time of Herophilus the presence of the glands and associated ducts had been described.[21] Around the time of the early 17th century the word used to describe the vesicles, parastatai, eventually and unambiguously was used to refer to the prostate gland, rather than the vesicles.[21] The first time the prostate was portrayed in an individual drawing was by Reiner De Graaf in 1678.[21]
The first described use of laparoscopic surgery on the vesicles was described in 1993; this is now the preferred approach because of decreased pain, complications, and a shorter hospital stay.[8]
Additional images
-
Seminal vesicles seen on an MRI scan through the pelvis. The large cyan-coloured area is the bladder, and the lobulated smaller structures below it are the vesicles.
-
Seminal vesicles seen in a cadaveric specimen from on top, with the bladder to the bottom of the image, and the rectum at the top. Their position near the vas deferentia can be seen.
-
Fundus of the bladder with the vesiculae seminales.
See also
- Male accessory gland infection (MAGI)
- Ejaculatory duct
- Urethra
- Prostate
- List of distinct cell types in the adult human body
References
- ISBN 978-0-8138-1394-3.
- ^ ISBN 978-0781772006.
- ^ )
- ^ ISBN 9781496383907.
- ISBN 978-3-642-46018-0.
- ^ PMID 11753468.
- ^ ISBN 9780702047473.
- ^ ISBN 9781119245193.)
{{cite book}}:|last1=has generic name (help)CS1 maint: multiple names: authors list (link - ^ ISBN 978-1-4557-7016-8.
- ISBN 978-0323078429.
- ^ Dagur G, Warren K, Suh Y, Singh N, Khan SA. Detecting diseases of neglected seminal vesicles using imaging modalities: A review of current literature. Int J Reprod Biomed. 2016;14(5):293-302.
- ^ ISBN 978-1550093650.
- ^ a b c "Seminal vesicle diseases". Geneva Foundation for Medical Education and Research. Archived from the original on 2014-04-26.
- ^ "Is seminal vesiculitis a discrete disease entity? Clinical and microbiological study of seminal vesiculitis in patients with acute epididymitis". 4 July 2023.
- ISBN 9781901865042.
- PMID 21696400.
- PMID 24391141.
- ^ PMID 27072175.
- ^ ISBN 9781260092042.
- ISBN 978-0-521-33792-2.
- ^ S2CID 44922919.
The humor produced in those glandular bodies is poured into the urinary passage in the male along with semen and its uses are to excite to the sexual act, to make coitus pleasurable, and to moisten the urinary passageway.
- ^ Dixson, Alan F. "Sexual selection and evolution of the seminal vesicles in primates." Folia Primatologica 69.5 (1998): 300-306.
External links
- Histology image: 17501loa – Histology Learning System at Boston University - "Male Reproductive System: prostate, seminal vesicle"
- Anatomy photo:44:04-0202 at the SUNY Downstate Medical Center - "The Male Pelvis: The Urinary Bladder"
- Anatomy photo:44:08-0103 at the SUNY Downstate Medical Center - "The Male Pelvis: Structures Located Posterior to the Urinary Bladder"