Gluconeogenesis
Gluconeogenesis (GNG) is a metabolic pathway that results in the biosynthesis of glucose from certain non-carbohydrate carbon substrates. It is a ubiquitous process, present in plants, animals, fungi, bacteria, and other microorganisms.[1] In vertebrates, gluconeogenesis occurs mainly in the liver and, to a lesser extent, in the cortex of the kidneys. It is one of two primary mechanisms – the other being degradation of glycogen (glycogenolysis) – used by humans and many other animals to maintain blood sugar levels, avoiding low levels (hypoglycemia).[2] In ruminants, because dietary carbohydrates tend to be metabolized by rumen organisms, gluconeogenesis occurs regardless of fasting, low-carbohydrate diets, exercise, etc.[3] In many other animals, the process occurs during periods of fasting, starvation, low-carbohydrate diets, or intense exercise.
In humans, substrates for gluconeogenesis may come from any non-carbohydrate sources that can be converted to
The gluconeogenesis pathway is highly
Precursors
In humans the main gluconeogenic precursors are lactate, glycerol (which is a part of the triglyceride molecule), alanine and glutamine. Altogether, they account for over 90% of the overall gluconeogenesis.[8] Other
In ruminants, propionate is the principal gluconeogenic substrate.[3][11] In nonruminants, including human beings, propionate arises from the β-oxidation of odd-chain and branched-chain fatty acids, and is a (relatively minor) substrate for gluconeogenesis.[12][13]
Lactate is transported back to the liver where it is converted into
Whether even-chain
The existence of the glyoxylate cycle in humans has not been established, and it is widely held that fatty acids cannot be converted to glucose in humans directly.
Location
In mammals, gluconeogenesis has been believed to be restricted to the liver,[20] the kidney,[20] the intestine,[21] and muscle,[22] but recent evidence indicates gluconeogenesis occurring in astrocytes of the brain.[23] These organs use somewhat different gluconeogenic precursors. The liver preferentially uses lactate, glycerol, and glucogenic amino acids (especially alanine) while the kidney preferentially uses lactate, glutamine and glycerol.[24][8] Lactate from the Cori cycle is quantitatively the largest source of substrate for gluconeogenesis, especially for the kidney.[8] The liver uses both glycogenolysis and gluconeogenesis to produce glucose, whereas the kidney only uses gluconeogenesis.[8] After a meal, the liver shifts to glycogen synthesis, whereas the kidney increases gluconeogenesis.[10] The intestine uses mostly glutamine and glycerol.[21]
Propionate is the principal substrate for gluconeogenesis in the ruminant liver, and the ruminant liver may make increased use of gluconeogenic amino acids (e.g., alanine) when glucose demand is increased.[25] The capacity of liver cells to use lactate for gluconeogenesis declines from the preruminant stage to the ruminant stage in calves and lambs.[26] In sheep kidney tissue, very high rates of gluconeogenesis from propionate have been observed.[26]
In all species, the formation of
Pathway
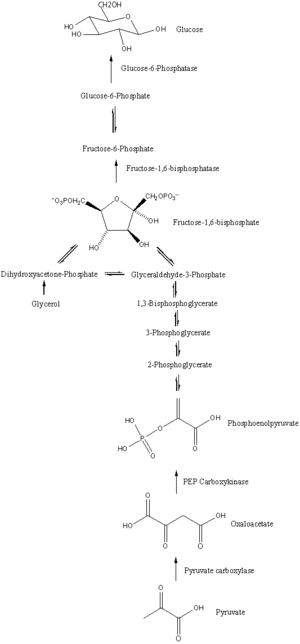
Gluconeogenesis is a pathway consisting of a series of eleven enzyme-catalyzed reactions. The pathway will begin in either the liver or kidney, in the mitochondria or cytoplasm of those cells, this being dependent on the substrate being used. Many of the reactions are the reverse of steps found in glycolysis.[citation needed]
- Gluconeogenesis begins in the mitochondria with the formation of oxaloacetate by the carboxylation of pyruvate. This reaction also requires one molecule of β-oxidationin the liver) and inhibited by high levels of ADP and glucose.
- Oxaloacetate is reduced to malate using NADH, a step required for its transportation out of the mitochondria.
- Malate is oxidized to oxaloacetate using NAD+ in the cytosol, where the remaining steps of gluconeogenesis take place.
- Oxaloacetate is decarboxylated and then phosphorylated to form during this reaction.
- The next steps in the reaction are the same as reversed glycolysis. However, fructose 1,6-bisphosphatase converts fructose 1,6-bisphosphate to fructose 6-phosphate, using one water molecule and releasing one phosphate (in glycolysis, phosphofructokinase 1 converts F6P and ATP to F1,6BP and ADP). This is also the rate-limiting step of gluconeogenesis.
- phosphoglucoisomerase(the reverse of step 2 in glycolysis). Glucose-6-phosphate can be used in other metabolic pathways or dephosphorylated to free glucose. Whereas free glucose can easily diffuse in and out of the cell, the phosphorylated form (glucose-6-phosphate) is locked in the cell, a mechanism by which intracellular glucose levels are controlled by cells.
- The final gluconeogenesis, the formation of glucose, occurs in the glucose-6-phosphatase to produce glucose and release an inorganic phosphate. Like two steps prior, this step is not a simple reversal of glycolysis, in which hexokinase catalyzes the conversion of glucose and ATP into G6P and ADP. Glucose is shuttled into the cytoplasm by glucose transporterslocated in the endoplasmic reticulum's membrane.
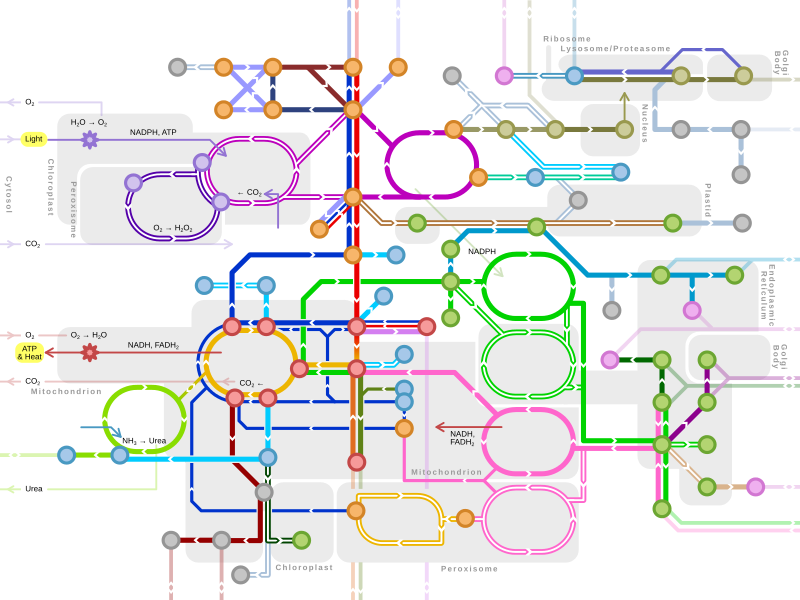
| Metabolism of common monosaccharides, including glycolysis, gluconeogenesis, glycogenesis and glycogenolysis |
|---|
 |
Regulation
While most steps in gluconeogenesis are the reverse of those found in
The majority of the
Global control of gluconeogenesis is mediated by glucagon (released when blood glucose is low); it triggers phosphorylation of enzymes and regulatory proteins by Protein Kinase A (a cyclic AMP regulated kinase) resulting in inhibition of glycolysis and stimulation of gluconeogenesis. Insulin counteracts glucagon by inhibiting gluconeogenesis. Type 2 diabetes is marked by excess glucagon and insulin resistance from the body.[30] Insulin can no longer inhibit the gene expression of enzymes such as PEPCK which leads to increased levels of hyperglycemia in the body.[31] The anti-diabetic drug metformin reduces blood glucose primarily through inhibition of gluconeogenesis, overcoming the failure of insulin to inhibit gluconeogenesis due to insulin resistance.[32]
Studies have shown that the absence of hepatic glucose production has no major effect on the control of fasting plasma glucose concentration. Compensatory induction of gluconeogenesis occurs in the kidneys and intestine, driven by
Insulin resistance
In the liver, the FOX protein FOXO6 normally promotes gluconeogenesis in the fasted state, but insulin blocks FOXO6 upon feeding.[34] In a condition of insulin resistance, insulin fails to block FOXO6 resulting in continued gluconeogenesis even upon feeding, resulting in high blood glucose (hyperglycemia).[34]
Insulin resistance is a common feature of
Origins
Gluconeogenesis is considered one of the most ancient anabolic pathways and is likely to have been exhibited in the last universal common ancestor.[36] Rafael F. Say and Georg Fuchs stated in 2010 that "all archaeal groups as well as the deeply branching bacterial lineages contain a bifunctional fructose 1,6-bisphosphate (FBP) aldolase/phosphatase with both FBP aldolase and FBP phosphatase activity. This enzyme is missing in most other Bacteria and in Eukaryota, and is heat-stabile even in mesophilic marine Crenarchaeota". It is proposed that fructose 1,6-bisphosphate aldolase/phosphatase was an ancestral gluconeogenic enzyme and had preceded glycolysis.[37] But the chemical mechanisms between gluconeogenesis and glycolysis, whether it is anabolic or catabolic, are similar, suggesting they both originated at the same time. Fructose 1,6-bisphosphate is shown to be nonenzymatically synthesized continuously within a freezing solution. The synthesis is accelerated in the presence of amino acids such as glycine and lysine implying that the first anabolic enzymes were amino acids. The prebiotic reactions in gluconeogenesis can also proceed nonenzymatically at dehydration-desiccation cycles. Such chemistry could have occurred in hydrothermal environments, including temperature gradients and cycling of freezing and thawing. Mineral surfaces might have played a role in the phosphorylation of metabolic intermediates from gluconeogenesis and have to been shown to produce tetrose, hexose phosphates, and pentose from formaldehyde, glyceraldehyde, and glycolaldehyde.[38][39][40]
See also
References
- ISBN 978-1-57259-153-0.
- ^ Silva P. "The Chemical Logic Behind Gluconeogenesis". Archived from the original on August 26, 2009. Retrieved September 8, 2009.
- ^ ISBN 978-0801442384.
- ^ PMID 21814506.
- S2CID 53097552.
- ISBN 978-0-07-182537-5.
- ISBN 978-0-7817-2265-0.
- ^ PMID 11213896.
- ^ ISBN 978-0-03-097369-7.
- ^ S2CID 24330397.
- ISBN 978-1501732355.
- ^ Rodwell VW, Bender DA, Botham KM, Kennelly PJ, Weil PA (2018). Harper's Illustrated Biochemistry (31st ed.). McGraw-Hill Publishing Company.
- ^ Baynes J, Dominiczak M (2014). Medical Biochemistry (4th ed.). Elsevier.
- ^ PMID 9725823.
- ^ PMID 19117076.
- PMID 7781887.
- ^ PMID 17059607.
- PMID 13441426.
- PMID 438326.
- ^ ISBN 978-0-07-282741-5.
- ^ PMID 15302872.
- PMID 25511375.
- PMID 28101056.
- PMID 20546255.
- PMID 10438042.
- ^ PMID 7601789.
- ^ ISBN 978-0-470-12930-2.
- ^ Christos Chinopoulos (2020), From Glucose to Lactate and Transiting Intermediates Through Mitochondria, Bypassing Pyruvate Kinase: Considerations for Cells Exhibiting Dimeric PKM2 or Otherwise Inhibited Kinase Activity, https://www.frontiersin.org/articles/10.3389/fphys.2020.543564/full
- S2CID 633399.
- PMID 19450513.
- PMID 28868790.
- PMID 29115403.
- PMID 22013018.
- ^ PMID 28213398.
- KiB)
- PMID 30538225.
- S2CID 4343445.
- S2CID 220671580.
- PMID 28652321.
- PMID 30166494.