Crohn's disease
| Crohn's disease | |
|---|---|
| Other names | Crohn disease, Crohn syndrome, granulomatous enteritis, regional enteritis, Leśniowski-Crohn disease |
| Prognosis | Slightly increased risk of death[11] |
| Frequency | 3.2 per 1,000 (developed world)[12] |
| Named after | |
Crohn's disease is a type of
Although the precise causes of Crohn's disease (CD) are unknown, it is believed to be caused by a combination of environmental,
About half of the overall risk is related to genetics, with more than 70 genes involved.[1][20] Tobacco smokers are three times as likely to develop Crohn's disease as non-smokers.[6] It often begins after gastroenteritis.[1] Other conditions with similar symptoms include irritable bowel syndrome and Behçet's disease.[1]
There is no known cure for Crohn's disease.
Crohn's disease affects about 3.2 per 1,000 people in Europe and North America;
Name controversy
The disease was named after
Signs and symptoms
| Crohn's disease | Ulcerative colitis | |
|---|---|---|
| Defecation | Often porridge-like,[31] sometimes steatorrhea |
Often mucus-like and with blood[31] |
| Tenesmus | Less common[31] | More common[31] |
| Fever | Common[31] | Indicates severe disease[31] |
| Fistulae | Common[32] | Seldom |
| Weight loss | Often | More seldom |
Gastrointestinal
Many people with Crohn's disease have symptoms for years before the diagnosis.
Perianal
Intestines
The intestines, especially the colon and terminal ileum, are the areas of the body affected most commonly.
Stomach and esophagus
The stomach is rarely the sole or predominant site of CD. To date there are only a few documented case reports of adults with isolated gastric CD and no reports in the pediatric population. Isolated stomach involvement is very unusual presentation accounting for less than 0.07% of all gastrointestinal CD.[40] Rarely, the esophagus and stomach may be involved in Crohn's disease. These can cause symptoms including difficulty swallowing (dysphagia), upper abdominal pain, and vomiting.[41]
Oropharynx (mouth)
The mouth may be affected by recurrent sores (
People with Crohn's disease are also susceptible to
Systemic
Like many other chronic, inflammatory diseases, Crohn's disease can cause a variety of
Extraintestinal
Crohn's disease can affect many organ systems beyond the gastrointestinal tract.[47]
| Crohn's disease |
Ulcerative colitis | ||
|---|---|---|---|
| Nutrient deficiency | Higher risk | ||
Colon cancer risk |
Slight | Considerable | |
| Prevalence of extraintestinal complications[48][49][50] | |||
Iritis/uveitis |
Females | 2.2% | 3.2% |
| Males | 1.3% | 0.9% | |
| Primary sclerosing cholangitis |
Females | 0.3% | 1% |
| Males | 0.4% | 3% | |
| Ankylosing spondylitis |
Females | 0.7% | 0.8% |
| Males | 2.7% | 1.5% | |
| Pyoderma gangrenosum |
Females | 1.2% | 0.8% |
| Males | 1.3% | 0.7% | |
| Erythema nodosum | Females | 1.9% | 2% |
| Males | 0.6% | 0.7% | |
Visual
Inflammation of the interior portion of the eye, known as uveitis, can cause blurred vision and eye pain, especially when exposed to light (photophobia).[51] Uveitis can lead to loss of vision if untreated.[47]
Inflammation may also involve the white part of the eye (
Other very rare ophthalmological manifestations include: conjunctivitis, glaucoma, and retinal vascular disease.[52]
Gallbladder and liver
Crohn's disease that affects the ileum may result in an increased risk of gallstones. This is due to a decrease in bile acid resorption in the ileum, and the bile gets excreted in the stool. As a result, the cholesterol/bile ratio increases in the gallbladder, resulting in an increased risk for gallstones.[51] Although the association is greater in the context of ulcerative colitis, Crohn's disease may also be associated with primary sclerosing cholangitis, a type of inflammation of the bile ducts.[53]
Liver involvement of Crohn's disease can include
Other rare hepatobiliary manifestations of Crohn's disease include: cholangiocarcinoma, granulomatous hepatitis, cholelithiasis, autoimmune hepatitis, hepatic abscess, and pericholangitis.[52]
Renal and urological
Urological manifestations in patients with IBD may include ureteral calculi, enterovesical fistula, perivesical infection, perinephric abscess, and obstructive uropathy with hydronephrosis. Ureteral compression is associated with retroperitoneal extension of the phlegmonous inflammatory process involving the terminal ileum and cecum, and may result in hydronephrosis severe enough to cause hypertension.[52]
Immune complex glomerulonephritis presenting with proteinuria and hematuria has been described in children and adults with CD or UC. Diagnosis is by renal biopsy, and treatment parallels the underlying IBD.[52]
Amyloidosis (see endocrinological involvement) secondary to Crohn's disease has been described and is known to affect the kidneys.[52]
Pancreatic
Pancreatitis may be associated with both UC and CD. The most common cause is iatrogenic and involves sensitivity to medications used to treat IBD (3% of patients), including sulfasalazine, mesalamine, 6-mercaptopurine, and azathioprine. Pancreatitis may present as symptomatic (in 2%) or more commonly asymptomatic (8–21%) disease in adults with IBD.[52]
Cardiovascular and circulatory
Children and adults with IBD have been rarely (<1%) reported developing pleuropericarditis either at initial presentation or during active or quiescent disease. The pathogenesis of pleuropericarditis is unknown, although certain medications (e.g., sulfasalazine and mesalamine derivatives) have been implicated in some cases. The clinical presentation may include chest pain, dyspnea, or in severe cases pericardial tamponade requiring rapid drainage. Nonsteroidal anti-inflammatory drugs have been used as therapy, although this should be weighed against the hypothetical risk of exacerbating the underlying IBD.[52]
In rare cases, cardiomyopathy, endocarditis, and myocarditis have been described.[52]
Crohn's disease also increases the risk of
Respiratory
Considering extraintestinal manifestations of CD, those involving the lung are relatively rare. However, there is a wide array of lung manifestations, ranging from subclinical alterations, airway diseases and lung parenchymal diseases to pleural diseases and drug-related diseases. The most frequent manifestation is bronchial inflammation and suppuration with or without bronchiectasis. There are a number of mechanisms by which the lungs may become involved in CD. These include the same embryological origin of the lung and gastrointestinal tract by ancestral intestine, similar immune systems in the pulmonary and intestinal mucosa, the presence of circulating immune complexes and auto-antibodies, and the adverse pulmonary effects of some drugs.[57] A complete list of known pulmonary manifestations include: fibrosing alveolitis, pulmonary vasculitis, apical fibrosis, bronchiectasis, bronchitis, bronchiolitis, tracheal stenosis, granulomatous lung disease, and abnormal pulmonary function.[52]
Musculoskeletal
Crohn's disease is associated with a type of rheumatologic disease known as seronegative spondyloarthropathy.[51] This group of diseases is characterized by inflammation of one or more joints (arthritis) or muscle insertions (enthesitis).[51] The arthritis in Crohn's disease can be divided into two types. The first type affects larger weight-bearing joints such as the knee (most common), hips, shoulders, wrists, or elbows.[51] The second type symmetrically involves five or more of the small joints of the hands and feet.[51] The arthritis may also involve the spine, leading to ankylosing spondylitis if the entire spine is involved, or simply sacroiliitis if only the sacroiliac joint is involved.[51]
Crohn's disease increases the risk of osteoporosis or thinning of the bones.[51] Individuals with osteoporosis are at increased risk of bone fractures.[58]
Dermatological

Crohn's disease may also involve the skin, blood, and
Pyoderma gangrenosum is a less common skin problem, occurring in under 2%,[60] and is typically a painful ulcerating nodule.[59][47]
Clubbing, a deformity of the ends of the fingers, may also be a result of Crohn's disease.[citation needed]
Other very rare dermatological manifestations include:
Neurological
Crohn's disease can also cause
Central and peripheral neurological disorders are described in patients with IBD and include peripheral neuropathies, myopathies, focal central nervous system defects, convulsions, confusional episodes, meningitis, syncope, optic neuritis, and sensorineural loss. Autoimmune mechanisms are proposed for involvement with IBD. Nutritional deficiencies associated with neurological manifestations, such as vitamin B12 deficiency, should be investigated. Spinal abscess has been reported in both a child and an adult with initial complaints of severe back pain due to extension of a psoas abscess from the epidural space to the subarachnoid space.[52]
Psychiatric and psychological
Crohn's disease is linked to many psychological disorders, including depression and anxiety, denial of one's disease, the need for dependence or dependent behaviors, feeling overwhelmed, and having a poor self-image.[62]
Many studies have found that patients with IBD report a higher frequency of depressive and anxiety disorders than the general population; most studies confirm that women with IBD are more likely than men to develop affective disorders and show that up to 65% of them may have depression and anxiety disorder.[63][64]
Endocrinological or hematological
Secondary amyloidosis (AA) is another rare but serious complication of inflammatory bowel disease (IBD), generally seen in Crohn's disease. At least 1% of patients with Crohn's disease develop amyloidosis. In the literature, the time lapse between the onset of Crohn's disease and the diagnosis of amyloidosis has been reported to range from 1 to 21 years.
In rare cases, hypercoagulation disorders and portal vein thrombosis have been described.[52]
Malnutrition symptoms
People with Crohn's disease may develop anemia due to
Complications
Intestinal damage

Crohn's disease can lead to several mechanical complications within the
Symptoms caused by
Intestinal granulomas are a walled-off portions of the intestine by macrophages in order to isolate infections. Granuloma formation is more often seen in younger patients, and mainly in the severe, active penetrating disease.[73] Granuloma is considered the hallmark of microscopic diagnosis in Crohn's disease (CD), but granulomas can be detected in only 21–60% of CD patients.[73]
Cancer
Crohn's disease also increases the risk of
Some studies suggest there is a role for chemoprotection in the prevention of colorectal cancer in Crohn's involving the colon; two agents have been suggested,
Some cancers, such as acute myelocytic leukaemia have been described in cases of Crohn's disease.[52] Hepatosplenic T-cell lymphoma (HSTCL) is a rare, lethal disease generally seen in young male patients with inflammatory bowel disease. TNF-α Inhibitor treatments (infliximab, adalimumab, certolizumab, natalizumab, and etanercept) are thought to be the cause of this rare disease.[79]

Major complications
Major complications of Crohn's disease include
Other complications
Individuals with Crohn's disease are at risk of
Pregnancy
Crohn's disease can be problematic during
Common complications of an
Etiology
The
Autoinflammatory theory
Crohn's disease can be described as a multifactorial autoinflammatory disease. The etiopathogenesis of Crohn's disease is still unknown. In any event, a loss of the regulatory capacity of the immune apparatus would be implicated in the onset of the disease. In this respect interestingly enough, as for
Some examples of how the innate immune system affects bowel inflammation have been described.
The thinking is that because Crohn's disease has strong innate immune system involvement and has NOD2 mutations as a predisposition, Crohn's disease is more likely an autoinflammatory disease than an autoimmune disease.[87]
Immunodeficiency theory
A substantial body of data has emerged in recent years to suggest that the primary defect in Crohn's disease is actually one of relative
Risk factors
| Crohn's disease | Ulcerative colitis | |
|---|---|---|
| Smoking | Higher risk for smokers | Lower risk for smokers[90] |
| Age | Usual onset between 15 and 30 years[91] |
Peak incidence between 15 and 25 years |
While the exact cause or causes are unknown, Crohn's disease seems to be due to a combination of environmental factors and genetic predisposition.[92] Crohn's is the first genetically complex disease in which the relationship between genetic risk factors and the immune system is understood in considerable detail.[93] Each individual risk mutation makes a small contribution to the overall risk of Crohn's (approximately 1:200). The genetic data, and direct assessment of immunity, indicates a malfunction in the innate immune system.[94] In this view, the chronic inflammation of Crohn's is caused when the adaptive immune system tries to compensate for a deficient innate immune system.[95]
Genetics
Crohn's has a genetic component.[97] Because of this, siblings of known people with Crohn's are 30 times more likely to develop Crohn's than the general population.[98]
The first mutation found to be associated with Crohn's was a
Crohn's has been linked to the gene
Immune system
There was a prevailing view that Crohn's disease is a primary
In 2007, the ATG16L1 gene was implicated in Crohn's disease, which may induce
Microbes
It is hypothesized that maintenance of
There is an apparent connection between Crohn's disease,
NOD2 is a gene involved in Crohn's genetic susceptibility. It is associated with
Other studies have linked specific strains of enteroadherent E. coli to the disease.[125] Adherent-invasive Escherichia coli (AIEC), more common in people with CD,[126][127][125] have the ability to make strong biofilms compared to non-AIEC strains correlating with high adhesion and invasion indices[128][129] of neutrophils and the ability to block autophagy at the autolysosomal step, which allows for intracellular survival of the bacteria and induction of inflammation.[130] Inflammation drives the proliferation of AIEC and dysbiosis in the ileum, irrespective of genotype.[131] AIEC strains replicate extensively inside macrophages inducing the secretion of very large amounts of TNF-α.[132]
Mouse studies have suggested some symptoms of Crohn's disease, ulcerative colitis, and irritable bowel syndrome have the same underlying cause. Biopsy samples taken from the colons of all three patient groups were found to produce elevated levels of a serine protease.[133] Experimental introduction of the serine protease into mice has been found to produce widespread pain associated with irritable bowel syndrome, as well as colitis, which is associated with all three diseases.[134] Regional and temporal variations in those illnesses follow those associated with infection with the protozoan Blastocystis.[135]
The "cold-chain" hypothesis is that
There is also a tentative association between Candida colonization and Crohn's disease.[139]
Still, these relationships between specific pathogens and Crohn's disease remain unclear.[140][141]
Environmental factors
The increased incidence of Crohn's in the
Those who consume vegetable proteins appear to have a lower incidence of Crohn's disease. Consumption of fish protein has no association.[142] Smoking increases the risk of the return of active disease (flares).[6] The introduction of hormonal contraception in the United States in the 1960s is associated with a dramatic increase in incidence, and one hypothesis is that these drugs work on the digestive system in ways similar to smoking.[143] Isotretinoin is associated with Crohn's.[144][145][146]Although
Pathophysiology
| Crohn's disease | Ulcerative colitis | |
|---|---|---|
| Cytokine response | Associated with Th17[153] |
Vaguely associated with Th2
|
During a colonoscopy, biopsies of the colon are often taken to confirm the diagnosis. Certain characteristic features of the pathology seen point toward Crohn's disease; it shows a transmural pattern of inflammation, meaning the inflammation may span the entire depth of the intestinal wall.[1]
Granulomas, aggregates of macrophage derivatives known as giant cells, are found in 50% of cases and are most specific for Crohn's disease. The granulomas of Crohn's disease do not show "caseation", a cheese-like appearance on microscopic examination characteristic of granulomas associated with infections, such as tuberculosis. Biopsies may also show chronic mucosal damage, as evidenced by blunting of the intestinal villi, atypical branching of the crypts, and a change in the tissue type (metaplasia). One example of such metaplasia, Paneth cell metaplasia, involves the development of Paneth cells (typically found in the small intestine and a key regulator of intestinal microbiota) in other parts of the gastrointestinal system.[154][155]
Diagnosis
The diagnosis of Crohn's disease can sometimes be challenging,
-
Endoscopic image of Crohn's colitis showing deep ulceration
-
CT scan showing Crohn's disease in the fundus of the stomach
-
Section of colectomy showing transmural inflammation
-
Resected ileum from a person with Crohn's disease
Classification
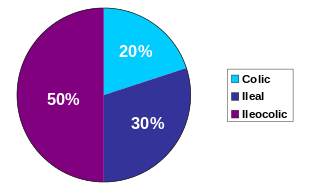
Crohn's disease is one type of inflammatory bowel disease (IBD). It typically manifests in the gastrointestinal tract and can be categorized by the specific tract region affected.
Gastroduodenal Crohn's disease causes inflammation in the stomach and the first part of the small intestine called the duodenum. Jejunoileitis causes spotty patches of inflammation in the top half of the small intestine, called the jejunum.[158] The disease can attack any part of the digestive tract, from mouth to anus. However, individuals affected by the disease rarely fall outside these three classifications, with presentations in other areas.[1]
Crohn's disease may also be categorized by the behavior of disease as it progresses. These categorizations formalized in the Vienna classification of the disease.
Endoscopy
A
Radiologic tests
A
Blood tests
A complete blood count may reveal anemia, which commonly is caused by blood loss leading to iron deficiency or by vitamin B12 deficiency, usually caused by ileal disease impairing vitamin B12 absorption. Rarely autoimmune hemolysis may occur.[170] Ferritin levels help assess if iron deficiency is contributing to the anemia. Erythrocyte sedimentation rate (ESR) and C-reactive protein help assess the degree of inflammation, which is important as ferritin can also be raised in inflammation.[171]
Other causes of anemia include medication used in treatment of inflammatory bowel disease, like azathioprine, which can lead to cytopenia, and sulfasalazine, which can also result in folate deficiency. Testing for Saccharomyces cerevisiae antibodies (ASCA) and antineutrophil cytoplasmic antibodies (ANCA) has been evaluated to identify inflammatory diseases of the intestine[172] and to differentiate Crohn's disease from ulcerative colitis.[173] Furthermore, increasing amounts and levels of serological antibodies such as ASCA, antilaminaribioside [Glc(β1,3)Glb(β); ALCA], antichitobioside [GlcNAc(β1,4)GlcNAc(β); ACCA], antimannobioside [Man(α1,3)Man(α)AMCA], antiLaminarin [(Glc(β1,3))3n(Glc(β1,6))n; anti-L] and antichitin [GlcNAc(β1,4)n; anti-C] associate with disease behavior and surgery, and may aid in the prognosis of Crohn's disease.[174][175][176][177]
Low serum levels of vitamin D are associated with Crohn's disease.[178] Further studies are required to determine the significance of this association.[178]
Comparison with ulcerative colitis
The most common disease that mimics the symptoms of Crohn's disease is ulcerative colitis, as both are inflammatory bowel diseases that can affect the colon with similar symptoms. It is important to differentiate these diseases, since the course of the diseases and treatments may be different. In some cases, however, it may not be possible to tell the difference, in which case the disease is classified as indeterminate colitis.[1][37][38]
| Crohn's disease | Ulcerative colitis | |
|---|---|---|
Terminal ileum involvement |
Commonly | Seldom |
| Colon involvement | Usually | Always |
| Rectum involvement | Seldom | Usually (95%)[90] |
| Involvement around the anus |
Common[179] | Seldom |
| Bile duct involvement | No increase in rate of primary sclerosing cholangitis | Higher rate[180] |
| Distribution of disease | Patchy areas of inflammation (skip lesions) | Continuous area of inflammation[90] |
| Endoscopy | Deep geographic and serpiginous (snake-like) ulcers
|
Continuous ulcer |
| Depth of inflammation | May be transmural, deep into tissues[179][181] | Shallow, mucosal |
| Stenosis | Common | Seldom |
| Granulomas on biopsy | May have non- | Non-peri- intestinal crypt granulomas not seen[184]
|
Differential diagnosis
Other conditions with similar symptoms as Crohn's disease includes intestinal
Management
Crohn's disease |
Ulcerative colitis
| |
|---|---|---|
| Mesalazine | Less useful[189] | More useful[189] |
| Antibiotics | Effective in long-term[190] | Generally not useful[191] |
| Surgery | Often returns following removal of affected part |
Usually cured by removal of colon |
There is no cure for Crohn's disease and
Lifestyle changes
Certain lifestyle changes can reduce symptoms, including dietary adjustments, elemental diet, proper hydration, and smoking cessation. Recent reviews underlined the importance to adopt diets that are best supported by evidence, even if little is known about the impact of diets on these patients.[193][194] Diets that include higher levels of fiber and fruit are associated with reduced risk, while diets rich in total fats,
Medication
Acute treatment uses medications to treat any infection (normally
Medications used to treat the symptoms of Crohn's disease include
The gradual loss of blood from the gastrointestinal tract, as well as chronic inflammation, often leads to anemia, and professional guidelines suggest routinely monitoring for this.[206][207][208]
Immunosuppressant therapies, infection risks and vaccinations
Many patients affected by Crohn's disease need immunosuppressant therapies, which are known to be associated with a higher risk of contracting opportunistic infectious diseases and of pre-neoplastic or neoplastic lesions such as cervical high-grade dysplasia and cancer.[209][210] Many of these potentially harmful diseases, such as Hepatitis B, Influenza, chickenpox, herpes zoster virus, pneumococcal pneumonia, or human papilloma virus, can be prevented by vaccines. Each drug used in the treatment of IBD should be classified according to the degree of immunosuppression induced in the patient. Several guidelines suggest investigating patients’ vaccination status before starting any treatment and performing vaccinations against Vaccine-preventable disease when required.[211][212] Compared to the rest of the population, patients affected by IBD are known to be at higher risk of contracting some
Surgery
Crohn's cannot be cured by surgery, as the disease eventually recurs, though it is used in the case of partial or full blockage of the intestine.[216] Surgery may also be required for complications such as obstructions, fistulas, or abscesses, or if the disease does not respond to drugs. After the first surgery, Crohn's usually comes back at the site where the diseased intestine was removed and the healthy ends were rejoined; it can also come back in other locations. After a resection, scar tissue builds up, which can cause strictures, which form when the intestines become too small to allow excrement to pass through easily, which can lead to a blockage. After the first resection, another resection may be necessary within five years.[217] For patients with an obstruction due to a stricture, two options for treatment are strictureplasty and resection of that portion of bowel. There is no statistical significance between strictureplasty alone versus strictureplasty and resection in cases of duodenal involvement. In these cases, re-operation rates were 31% and 27%, respectively, indicating that strictureplasty is a safe and effective treatment for selected people with duodenal involvement.[218]
Postsurgical recurrence of Crohn's disease is relatively common. Crohn's lesions are nearly always found at the site of the resected bowel. The join (or anastomosis) after surgery may be inspected, usually during a colonoscopy, and disease activity graded. The "Rutgeert's score" is an endoscopic scoring system for postoperative disease recurrence in Crohn's disease. Mild postsurgical recurrences of Crohn's disease are graded i1 and i2, moderate to severe recurrences are graded i3 and i4.[219] Fewer lesions result in a lower grade. Based on the score, treatment plans can be designed to give the patient the best chance of managing the recurrence of the disease.[220]
Microbiome modification
The use of oral
Mental health
Crohn's may result in
As of 2017[update] there is a small amount of research looking at
Alternative medicine
It is common for people with Crohn's disease to try
- Acupuncture is used to treat inflammatory bowel disease in China, and is being used more frequently in Western society.[228] At this time, evidence is insufficient to recommend the use of acupuncture.[227]
- A 2006 survey in Germany found that about half of people with IBD used some form of alternative medicine, with the most common being
- There are contradicting studies regarding the effect of medical cannabis on inflammatory bowel disease,[236] and its effects on management are uncertain.[237]
Prognosis
Crohn's disease is a
Epidemiology
The percentage of people with Crohn's disease has been determined in
Crohn's disease begins most commonly in people in their teens and 20s, and people in their 50s through to their 70s.[1][37][26] It is rarely diagnosed in early childhood. It usually affects female children more severely than males.[245] However, only slightly more women than men have Crohn's disease.[246] Parents, siblings or children of people with Crohn's disease are 3 to 20 times more likely to develop the disease.[247] Twin studies find that if one has the disease there is a 55% chance the other will too.[248]
The incidence of Crohn's disease is increasing in Europe[249] and in newly industrialised countries.[250] For example, in Brazil, there has been an annual increase of 11% in the incidence of Crohn's disease since 1990.[250]
History
Inflammatory bowel diseases were described by Giovanni Battista Morgagni (1682–1771) and by Scottish physician Thomas Kennedy Dalziel in 1913.[251]
Ileitis terminalis was first described by Polish surgeon
References
- ^ PMID 22914295.
- ^ "Crohn's disease". Autoimmune Registry Inc. Archived from the original on June 15, 2022. Retrieved June 15, 2022.
- ^ a b c d e f g h i "Crohn's Disease". National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Archived from the original on December 8, 2019. Retrieved December 8, 2019.
- ^ English: Baumgart DC, Carding SR. Inflammatory bowel disease: cause and immunobiology. Lancet. 2007;369:1627-1640.
- ^ English: Mawdsley JE, Rampton DS. Psychological stress in IBD: new insights into pathogenic and therapeutic implications. Gut. 2005;54:1481-1491.
- ^ PMID 15157822.
- S2CID 31528819. Archived from the original on June 13, 2019.)
{{cite journal}}: CS1 maint: date and year (link - ^ English: Frisch M, Gridley G.Appendectomy in adulthood and the risk of inflammatory bowel diseases.Scand J Gastroenterol. 2002;37:1175-1177.
- S2CID 2625962.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ a b c "Inflammatory Bowel Disease" (PDF). World Gastroenterology Organization. August 2015. Archived from the original (PDF) on March 14, 2016. Retrieved March 13, 2016.
- ^ S2CID 4568430.
- ^ from the original on October 7, 2022. Retrieved October 7, 2022.
- PMID 21530736.
- ^ PMID 18806708.
- PMID 18473770.
- ^ PMID 19437144.
- PMID 19687225.
- S2CID 25402952.
- PMID 17106921.
- PMID 18587394.
- S2CID 205468282.
- ^ PMID 22553396.
- ^ S2CID 9538639.
- PMID 27733281.
- S2CID 70796090.
- ^ a b c "Crohn's Disease: Get Facts on Symptoms and Diet". eMedicineHealth. Archived from the original on October 20, 2007.
- ^ PMID 10828911.
- PMID 31701137.
- S2CID 13714394.
- PMID 3514360.
- ^ a b c d e f internetmedicin.se > Inflammatorisk tarmsjukdom, kronisk, IBD By Robert Löfberg. Retrieved Oct 2010 Translate.
- S2CID 31219115.)
{{cite journal}}: CS1 maint: DOI inactive as of January 2024 (link - ^ S2CID 2764694.
- from the original on September 6, 2017. Retrieved August 30, 2017.
- S2CID 7831833.
- ^ a b "What I need to know about Crohn's Disease". www.niddk.nih.gov. Archived from the original on November 21, 2015. Retrieved December 11, 2015.
- ^ a b c d e f Crohn Disease at eMedicine
- ^ from the original on April 28, 2021. Retrieved September 4, 2018.
- S2CID 42383375.
- PMID 24303469.
- PMID 15605018.
- PMID 33477990.
- ^ PMID 28127561.
- ^ PMID 16632672.
- from the original on August 28, 2021. Retrieved September 4, 2018.
- PMID 8898436.
- ^ PMID 26614685.
- PMID 957999.
- PMID 11316157.
- PMID 26614685.
- ^ S2CID 10078879.
- ^ PMID 18223370.
- ISBN 978-0-7216-0187-8.
- from the original on October 7, 2022. Retrieved September 6, 2021.
- from the original on September 6, 2021. Retrieved September 6, 2021.
- S2CID 31002546.
- PMID 24415866.
- S2CID 28982700.
- ^ S2CID 1819416.
- ^ S2CID 59275029.
- ^ a b Crohn's disease Archived August 5, 2007, at the Wayback Machine. professionals.epilepsy.com. Retrieved July 13, 2007.
- ^ "Mental and Emotional Well-Being". Crohn's & Colitis Foundation. Archived from the original on October 7, 2022. Retrieved September 6, 2021.
- ^ Fracas E, Costantino A, Vecchi M, Buoli M. Depressive and Anxiety Disorders in Patients with Inflammatory Bowel Diseases: Are There Any Gender Differences? International Journal of Environmental Research and Public Health. 2023; 20(13):6255. https://doi.org/10.3390/ijerph20136255
- ^ Barberio B, Zamani M, Black CJ, Savarino EV, Ford AC. Prevalence of symptoms of anxiety and depression in patients with inflammatory bowel disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021 May;6(5):359-370. doi: 10.1016/S2468-1253(21)00014-5
- ^ PMID 21450124.
- ^ PMID 21564345.
- ^ MedlinePlus Encyclopedia: Small bowel bacterial overgrowth
- ^ PMID 19643023.license.
 Text was copied from this source, which is available under a Creative Commons Attribution 2.0 Generic (CC BY 2.0) Archived February 23, 2011, at the Wayback Machine
Text was copied from this source, which is available under a Creative Commons Attribution 2.0 Generic (CC BY 2.0) Archived February 23, 2011, at the Wayback Machine - ^ "Intestinal Obstruction". MERCK MANUAL Consumer Version. Archived from the original on July 10, 2016. Retrieved June 27, 2016.
- ^ "Anorectal Fistula". MERCK MANUAL Consumer Version. Archived from the original on July 10, 2016. Retrieved June 27, 2016.
- ^ "Anorectal Abscess". MERCK MANUAL Consumer Version. Archived from the original on June 14, 2016. Retrieved June 27, 2016.
- ^ Enterovesical Fistula at eMedicine
- ^ PMID 15918200.
- PMID 28922695.
- from the original on August 5, 2020. Retrieved September 4, 2018.
- PMID 15735438.
- PMID 18461651.
- PMID 27239106.
- from the original on October 3, 2021. Retrieved October 3, 2021.
- ^ Carrillo M (September 1, 1985). "Man of Many Problems Comes to City for Help". Richmond Times-Dispatch. Richmond, Virginia, USA. p. B1.
- ^ "Kay, Laura Lynn". Richmond Times-Dispatch. Richmond, Virginia, USA. April 3, 2014.
Loebenberg P (March 2, 2014). "Doris L. Johnson, 82, of Westminster". Carroll County Times. Westminster, Maryland, USA.
Berrier Jr R (December 31, 2013). "In memoriam: Dan Hodges Jr". The Roanoke Times. Roanoke, Virginia, USA.
"Cynthia Meredith Routt". Daily Press. Newport News, Virginia, USA. May 4, 2014. p. A11. - S2CID 195305419.
- Crohn's and Colitis Foundation of America. Archived from the originalon February 17, 2012. Retrieved November 7, 2009.
- ISBN 978-1-78984-186-2. Archivedfrom the original on October 7, 2022. Retrieved September 6, 2021.
- ^ "Definition of Autoimmunity & Autoimmune Disease - Autoimmune Disease | Johns Hopkins Pathology". pathology.jhu.edu. Archived from the original on October 3, 2021. Retrieved October 3, 2021.
- ^ PMID 24164192.
- ^ PMID 29358878.
- PMID 27717419, retrieved November 4, 2021
- ^ PMID 19437144.
- ^ S2CID 73473272.
- ^ Nachimuthu S. "Crohn's disease". eMedicineHealth. Archived from the original on December 9, 2019. Retrieved December 8, 2019.
- S2CID 2627465.
- PMID 18473763.
- ^ a b
Marks DJ, Harbord MW, MacAllister R, Rahman FZ, Young J, Al-Lazikani B, et al. (February 2006). "Defective acute inflammation in Crohn's disease: a clinical investigation". Lancet. 367 (9511): 668–78. S2CID 13898663.
- PMID 16890491.
- PMID 22319155.
- Crohn's and Colitis Foundation of America. April 16, 2007. Archived from the originalon May 2, 2007. Retrieved November 7, 2009.
- PMID 24913378.
- S2CID 205017657.
- PMID 11910337.
- PMID 18775308.
- PMID 19213688.
- PMID 15157828.
- ^ PMID 17484864.
- PMID 24223725.
- PMID 20106866.
- S2CID 11429585.
- PMID 23128233.
- S2CID 5196629.
Recent genome-wide association studies have shown that chronic inflammatory and autoimmune diseases are linked genetically to coeliac disease; for example, type 1 diabetes mellitus, Grave's disease and Crohn's disease.
- ^ Coghlan A (January 10, 2018). "A single gene can either raise or lower Crohn's disease risk". New Scientist. Archived from the original on November 9, 2020. Retrieved November 5, 2020.
- PMID 18161747.
- S2CID 37353838.
- PMID 17570211.
- ^ Velasquez-Manoff M (June 29, 2008). "The Worm Turns". The New York Times. Archived from the original on January 7, 2017.
- S2CID 3329677.
- S2CID 25518704.
- PMID 18070962.
- PMID 17919633.
- PMID 16306778.
- PMID 24966610.
- ^ "New insights into Crohn's Disease". Archived from the original on September 23, 2013.
- PMID 21734790.)
{{cite journal}}: CS1 maint: DOI inactive as of January 2024 (link - PMID 17317344.
- PMID 21990211.
- ^ PMID 18043660.
- PMID 17660846.
- PMID 15300573.
- PMID 23251695.
- PMID 19772580.
- PMID 23272151.
- PMID 22848538.
- S2CID 23564986.
- PMID 17304351.
- PMID 12414536.
- PMID 18937874.
- S2CID 10254395.
- ^ "Fridges blamed for Crohn's disease rise". Medical News Today. December 12, 2003. Archived from the original on January 3, 2009.
- S2CID 13271176.
- PMID 21802979.
- ^ "Possible links between Crohn's disease and Paratuberculosis" (PDF). European Commission Directorate-General Health & Consumer Protection. Archived from the original (PDF) on December 17, 2008. Retrieved November 7, 2009.
- PMID 9096189.
- ^ a b
Shoda R, Matsueda K, Yamato S, Umeda N (May 1996). "Epidemiologic analysis of Crohn disease in Japan: increased dietary intake of n-6 polyunsaturated fatty acids and animal protein relates to the increased incidence of Crohn disease in Japan". The American Journal of Clinical Nutrition. 63 (5): 741–5. PMID 8615358.
- ^
Lesko SM, Kaufman DW, Rosenberg L, Helmrich SP, Miller DR, Stolley PD, et al. (November 1985). "Evidence for an increased risk of Crohn's disease in oral contraceptive users". Gastroenterology. 89 (5): 1046–9. PMID 4043662.
- S2CID 27663573.
- PMID 15381956.
- S2CID 22216642. Archived from the originalon June 29, 2012. Retrieved November 1, 2010.
- PMID 15250815.
- PMID 15613257.
- PMID 17922962.
- S2CID 9418654.
- ^ S2CID 20085592.
- .
- PMID 17570211.
- ^ Crawford JM. "The Gastrointestinal tract, Chapter 17". In Cotran RS, Kumar V, Robbins SL. Robbins Pathologic Basis of Disease: 5th Edition. W.B. Saunders and Company, Philadelphia, 1994.
- PMID 22719822.
- ^ HCP: Pill Cam, Capsule Endoscopy, Esophageal Endoscopy Archived June 16, 2008, at the Wayback Machine
- S2CID 35892792.
- PMID 8244104.
- ^ PMID 10701144.
- S2CID 21302609.
- ^ PMID 16373764.
- S2CID 25684863.
- PMID 8428417.
- PMID 12122746.
- PMID 16356814.
- from the original on October 7, 2022. Retrieved May 18, 2022.
- PMID 16609136.
- PMID 19959525.
- PMID 23674768.
- S2CID 72099458.
- PMID 16630759.
- PMID 16341311.
- PMID 16099791.
- PMID 17456509.
- S2CID 6015339.
- S2CID 25021606.
- S2CID 32035337.
- ^ PMID 26348447.
- ^ S2CID 31219115.)
{{cite journal}}: CS1 maint: DOI inactive as of January 2024 (link - S2CID 260320940.
- S2CID 35264387.
- S2CID 36907992.
- S2CID 29476514.
- PMID 24942757.
- S2CID 16823218.
Both the endomysial antibody and tissue transglutaminase antibody have very high sensitivities (93% for both) and specificities (>99% and >98% respectively) for the diagnosis of typical coeliac disease with villous atrophy. (...) As the detection of at least partial villous atrophy was used to make a diagnosis of coeliac disease in the vast majority of studies, we can't assume that the same LRs apply to coeliac patients with lesser abnormality such as an increase in intraepithelial lymphocytes or electron-microscopic changes only. In fact, if such lesser abnormalities were used as criteria for diagnosing (and excluding) coeliac disease, the sensitivity of the tests could be lower (i.e. more false negatives), especially since a number of studies suggest that the EMA and tTG antibody tests are less sensitive with lesser degrees of mucosal abnormality
- PMID 18775218. Archived from the originalon March 19, 2016. Retrieved March 13, 2016.
Estos marcadores presentan en general una elevada sensibilidad y especificidad (cercanas al 90%) en presencia de atrofia marcada de las vellosidades intestinales. Sin embargo, muestran una notable disminución de la sensibilidad (del orden del 40-50%) en casos con atrofia vellositaria leve o cambios mínimos. These markers generally have high sensitivity and specificity (around 90%) in the presence of marked atrophy of the villi. However, they show a marked decrease in sensitivity (of the order of 40-50%) in cases with mild villous atrophy or minimal changes.
- PMID 24834166.
- PMID 24834157.
- ^ ISBN 0-7817-7153-6.
- PMID 20067425.
- PMID 19444096.
- ^ a b c Fries WS, Nazario B (May 16, 2007). "Crohn's Disease: 54 Tips to Help You Manage". WebMD. Archived from the original on February 8, 2008. Retrieved February 14, 2008.
- ^ Roncoroni L, Gori R, Elli L, Tontini GE, Doneda L, Norsa L, Cuomo M, Lombardo V, Scricciolo A, Caprioli F, Costantino A, Scaramella L, Vecchi M. Nutrition in Patients with Inflammatory Bowel Diseases: A Narrative Review. Nutrients. 2022 Feb 10;14(4):751
- ^ Ananthakrishnan AN, Kaplan GG, Bernstein CN, Burke KE, Lochhead PJ, Sasson AN, Agrawal M, Tiong JHT, Steinberg J, Kruis W, Steinwurz F, Ahuja V, Ng SC, Rubin DT, Colombel JF, Gearry R; International Organization for Study of Inflammatory Bowel Diseases. Lifestyle, behaviour, and environmental modification for the management of patients with inflammatory bowel diseases: an International Organization for Study of Inflammatory Bowel Diseases consensus. Lancet Gastroenterol Hepatol. 2022 Apr 26:S2468-1253(22)00021-8.
- S2CID 10337669.
- ISBN 978-1-60831-017-3.
- S2CID 743620.
- PMID 29338679.
- ^ "FDA Approves Cimzia to Treat Crohn's Disease" (Press release). Food and Drug Administration (FDA). April 22, 2008. Archived from the original on October 20, 2009. Retrieved November 5, 2009.
- ^ "Prescribing information ustekinumab" (PDF). FDA. Archived (PDF) from the original on October 18, 2020. Retrieved May 23, 2019.
- PMID 16267322.
- PMID 30068022.
- ^ "Discover RINVOQ® (upadacitinib)". RINVOQ. Archived from the original on May 18, 2023. Retrieved May 29, 2023.
- ISBN 978-0-19-856837-7.
- ^ PMID 27885650.
- S2CID 8269837.
- PMID 21561874.
- PMID 17985376.
- ^ Beaugerie, L.; Itzkowitz, S.H. Cancers complicating inflammatory bowel disease. N. Engl. J. Med. 2015, 372, 1441–1452
- ^ Toruner, M.; Loftus, E.V.; Harmsen, W.S.; Zinsmeister, A.R.; Orenstein, R.; Sandborn, W.J.; Colombel, J.; Egan, L.J. Risk factors for opportunistic infections in patients with inflammatory bowel disease. Gastroenterology 2008, 134, 929–936
- ^ Farraye, F.A.; Melmed, G.Y.; Lichtenstein, G.R.; Kane, S.V. ACG Clinical Guideline: Preventive Care in Inflammatory Bowel Disease. Am. J. Gastroenterol. 2017, 112, 241–258.
- ^ Kucharzik, T.; Ellul, P.; Greuter, T.; Rahier, J.F.; Verstockt, B.; Abreu, C.; Albuquerque, A.; Allocca, M.; Esteve, M.; Farraye, F.A.; et al. ECCO Guidelines on the Prevention, Diagnosis, and Management of Infections in Inflammatory Bowel Disease. J. Crohn’s Colitis 2021, 15, 879–913.
- ^ Ananthakrishnan, A.N.; McGinley, E.L. Infection-related hospitalizations are associated with increased mortality in patients with inflammatory bowel diseases. J. Crohn’s Colitis 2013, 7, 107–112.
- ^ Malhi, G.; Rumman, A.; Thanabalan, R.; Croitoru, K.; Silverberg, M.S.; Steinhart, A.H.; Nguyen, G.C. Vaccination in inflammatory bowel disease patients: Attitudes, knowledge, and uptake. J. Crohn’s Colitis 2015, 9, 439–444.
- ^ Costantino, A.; Michelon, M.; Noviello, D.; Macaluso, F.S.; Leone, S.; Bonaccorso, N.; Costantino, C.; Vecchi, M.; Caprioli, F., on behalf of AMICI Scientific Board. Attitudes towards Vaccinations in a National Italian Cohort of Patients with Inflammatory Bowel Disease. Vaccines 2023, 11, 1591.
- PMID 26034346.
- About.com. Archivedfrom the original on November 13, 2007. Retrieved February 14, 2008.
- S2CID 33628350.
- PMID 2394349.
- PMID 24917974.
- ^ "Short Bowel Syndrome". National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). July 2015. Archived from the original on December 9, 2019. Retrieved December 8, 2019.
- ^ Rhodes M (October 24, 2006). "Intestinal transplant for Crohn's disease". Everyday Health. Archived from the original on October 8, 2008. Retrieved March 22, 2009.
- PMID 5337211.
- PMID 32678465.
- ^ from the original on April 28, 2021. Retrieved September 4, 2018.
- PMID 28102860.
- ^ PMID 16481630.
the colitis activity index fell significantly in the treatment group compared to the sham acupuncture group. However, recruitment did not reach its target and the number of patients was small.
- S2CID 7852406.
- S2CID 207298246.
- from the original on October 29, 2017. Retrieved October 28, 2017.
- ISBN 978-0-226-05182-6.
Yet homeopathy is a paradigmatic example of pseudoscience. It is neither simply bad science nor science fraud, but rather profoundly departs from scientific method and theories while being described as scientific by some of its adherents (often sincerely).
- ISBN 978-1-4614-8540-7.
within the traditional medical community it is considered to be quackery
- PMID 12492603.
- S2CID 17939264.
- ^ "Evidence Check 2: Homeopathy - Science and Technology Committee". British House of Commons Science and Technology Committee. February 22, 2010. Archived from the original on September 19, 2015. Retrieved April 5, 2014.
- S2CID 25309621.
- PMID 30407616.
- ^ "Crohn's disease - Prognosis". University of Maryland Medical Centre. Archived from the original on August 29, 2012. Retrieved October 19, 2012.
- S2CID 25193522.
- ^ PMID 3250100.
- PMID 8726303.
- PMID 9014768.
- PMID 8491401.
- S2CID 10988974.
- Crohn's and Colitis Foundation of America. Archived from the originalon February 16, 2008.
- ^ "Who is affected by Crohn's disease". Healthwise. Archived from the original on January 23, 2009.
- PMID 9203931.
- PMID 3396969.
- PMID 23395397.
- ^ S2CID 32940.
- PMID 2980764.
- PMID 3047387.
Further reading
- Lichtenstein GR, Loftus EV, Isaacs KL, Regueiro MD, Gerson LB, Sands BE (April 2018). "ACG Clinical Guideline: Management of Crohn's Disease in Adults". Am. J. Gastroenterol. 113 (4): 481–517. PMID 29610508.
External links
- "Crohn's disease". MedlinePlus. U.S. National Library of Medicine.
 Media related to Crohn's disease at Wikimedia Commons
Media related to Crohn's disease at Wikimedia Commons



