Viloxazine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Qelbree, others |
| Other names | ICI-58834; SPN-812; SPN-809 |
| License data |
|
| Routes of administration | By mouth |
| Drug class | Norepinephrine reuptake inhibitor |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Protein binding | 76–82%[1] |
| Metabolism | Hydroxylation (CYP2D6), glucuronidation (UGT1A9, UGT2B15)[1] |
| Metabolites | 5-Hydroxyviloxazine glucuronide[1] |
| Elimination half-life | IR: 2–5 hours[2] ER: 7.02 ± 4.74 hours[1] |
| Excretion | Urine (~90%), feces (<1%)[1][3] |
| Identifiers | |
| |
JSmol) | |
| Chirality | Racemic mixture |
SMILES
| |
| |
| | |
Viloxazine, sold under the brand name Qelbree among others, is a
Viloxazine was first described by 1972
Medical uses
Attention deficit hyperactivity disorder
Viloxazine is indicated to treat attention deficit hyperactivity disorder (ADHD) in children age 6 to 12 years, adolescents age 13 to 17 years, and adults.[1]
Analyses of clinical trial data suggest that viloxazine produces moderate reductions in symptoms; it is about as effective as atomoxetine and methylphenidate but with fewer side effects.[7][8][16]
Depression
Viloxazine was previously marketed as an antidepressant for the treatment of major depressive disorder.[6][5] It was considered to be effective in mild to moderate as well as severe depression with or without co-morbid symptoms.[6] The typical dose range for depression was 100 to 400 mg per day in divided doses administered generally two to three times per day.[6]
Available forms
Viloxazine is available for ADHD in the form of 100, 150, and 200 mg extended-release capsules.[1] These capsules can be opened and sprinkled into food for easier administration.[1]
Side effects
The most common side effects include
There were three cases of seizure worldwide, and most animal studies (and clinical trials that included epilepsy patients) indicated the presence of anticonvulsant properties, so viloxazine is not completely contraindicated in patients with epilepsy.[20]
Interactions
Viloxazine increased plasma levels of phenytoin by an average of 37%.[21] It also was known to significantly increase plasma levels of theophylline and decrease its clearance from the body,[22] sometimes resulting in accidental overdose of theophylline.[23]
Pharmacology
Pharmacodynamics
Viloxazine acts as a
More recent research has found that the
Pharmacokinetics
Absorption
The
Distribution
The plasma protein binding of viloxazine is 76 to 82% over a concentration range of 0.5 to 10 μg/mL.[1]
Metabolism
The
Elimination
The elimination of viloxazine is mainly renal.[1] Approximately 90% of the dose is excreted in urine within 24 hours and less than 1% of the dose is recovered in feces.[1]
The
Chemistry
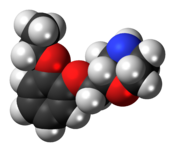
Viloxazine is a
History
Viloxazine was discovered by scientists at
The medication was first marketed in 1974.[6][10] Viloxazine was not approved for medical use by the FDA.[11] In 1984, the FDA granted the medication an orphan designation for treatment of cataplexy and narcolepsy with the tentative brand name Catatrol.[31] For unknown reasons however, it was never approved or introduced for these uses in the United States.[6] Viloxazine was withdrawn from markets worldwide in 2002 for commercial reasons unrelated to efficacy or safety.[6][12][13]
As of 2015, Supernus Pharmaceuticals was developing extended release formulations of viloxazine as a treatment for
The benefit of viloxazine was evaluated in three clinical studies, including two in children (ages 6 to 11 years) and one in adolescents (ages 12 to 17 years) with ADHD.[34] In each study, pediatric participants were randomly assigned to receive one of two doses of viloxazine or placebo once daily for 6 to 8 weeks.[34] None of the participants, their parent(s)/caregiver(s), the study sponsor, or the study doctors knew which treatment the participant received during the study.[34] The severity of ADHD symptoms observed at the last week of treatment was significantly greater in participants who received placebo compared with participants who received viloxazine.[34] The severity of ADHD symptoms was assessed using the Attention-Deficit Hyperactivity Disorder Rating Scale 5th Edition (ADHD-RS-5).[34] A fourth study provided information about the safety of viloxazine in adolescents 12 to 17 years of age with ADHD.[34] The FDA approved viloxazine based on evidence from several clinical trial(s) of 1289 participants with attention deficit hyperactivity disorder (ADHD).[34] The trials were conducted at 59 sites in the United States.[34]
Society and culture
Brand names
Viloxazine has been marketed under the brand names Emovit, Qelbree, Vicilan, Viloxazin, Viloxazina, Viloxazinum, Vivalan, and Vivarint.[6][35]
Research
Viloxazine has undergone two randomized controlled trials for nocturnal enuresis (bedwetting) in children, both of those times versus imipramine.[36][37] By 1990, it was seen as a less cardiotoxic alternative to imipramine, and to be especially effective in heavy sleepers.[38]
In narcolepsy, viloxazine has been shown to suppress auxiliary symptoms such as cataplexy and also abnormal sleep-onset REM[39] without significantly improving daytime somnolence.[40] In a cross-over trial (56 participants) viloxazine significantly reduced EDS and cataplexy.[13]
Viloxazine has also been studied for the treatment of alcoholism, with some success.[41]
Viloxazine did not demonstrate efficacy in a double-blind randomized controlled trial versus amisulpride in the treatment of dysthymia.[42]
References
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag "Qelbree- viloxazine hydrochloride capsule, extended release". DailyMed. Archived from the original on 28 October 2022. Retrieved 3 May 2022.
- ^ S2CID 44804763.
- PMID 1154799.
- ^ "SID 180462". PubChem Substance Summary. U.S. National Library of Medicine. Archived from the original on 14 June 2013. Retrieved 5 November 2005.
- ^ PMID 33121553.
- ^ PMID 34003459.)
{{cite journal}}: CS1 maint: overridden setting (link - ^ PMID 38824626.
- ^ S2CID 230716405.)
{{cite journal}}: CS1 maint: overridden setting (link - ^ S2CID 4268001.)
{{cite journal}}: CS1 maint: overridden setting (link - ^ PMID 10857386.
- ^ ISBN 9783540687061.
- ^ ISBN 9781609133450.
- ^ PMID 18254030.
- ^ a b "Qelbree: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). Archived from the original on 2 April 2021. Retrieved 2 April 2021.
- ^ a b "Supernus Announces FDA Approval of Qelbree (SPN-812) for the Treatment of ADHD". Supernus Pharmaceuticals (Press release). 2 April 2021. Archived from the original on 6 April 2021. Retrieved 3 April 2021.
- S2CID 104938.)
{{cite journal}}: CS1 maint: overridden setting (link - S2CID 221768208.
- PMID 9696909.
- S2CID 252258910.
- PMID 6434699.
- PMID 1538217.)
{{cite journal}}: CS1 maint: overridden setting (link - PMID 2815226.
- S2CID 10114046.
- ^ PMID 9537821.
- ^ PMID 32943948.
- PMID 6086881.
- PMID 3816971.
- ^ ISSN 1092-8529.
- PMID 6326891.
- ISBN 978352760749-5.
- ^ "Orphan Drug Designations and Approvals: Viloxazine". U.S. Food and Drug Administration. Archived from the original on 25 June 2022. Retrieved 1 August 2015.
- ^ "Supernus profile". Bloomberg. Archived from the original on 11 March 2018. Retrieved 1 August 2015.
- ^ "Psychiatry portfolio". Supernus. Archived from the original on 17 April 2016. Retrieved 1 August 2015.
- ^ a b c d e f g h "Drug Trials Snapshots: Qelbree". U.S. Food and Drug Administration. 13 March 2023. Archived from the original on 14 March 2023. Retrieved 13 March 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ISBN 978-3-88763-075-1. Archivedfrom the original on 14 January 2023. Retrieved 3 May 2022.
- PMID 6364124.
- PMID 3332732.
- PMID 2371930.
- PMID 3704453.
- PMID 1968069.
- PMID 2079386.
- from the original on 13 October 2022. Retrieved 24 September 2019.
External links
- Clinical trial number NCT03247530 for "Evaluation of SPN-812 ER Low Dose in Children With ADHD" at ClinicalTrials.gov
- Clinical trial number NCT03247543 for "Evaluation of SPN-812 ER High Dose in Children With ADHD" at ClinicalTrials.gov
